Introduction
Multidrug-resistant Gram-negative bacteria cause infections that are difficult to treat and associated with high mortality rates. Such infections are a major problem in Türkiye and worldwide (1,2). The carbapenem group of antibiotics is commonly used in infections caused by resistant Gram-negative microorganisms. However, the frequent use of carbapenems has caused more serious issues, including the emergence of carbapenem-resistant Enterobacterales (CRE), carbapenem-resistant Pseudomonas aeruginosa (CRPA), and carbapenem-resistant Acinetobacter baumannii (CRAB) (3). The mortality rates of these infections are higher than those caused by carbapenem-susceptible pathogens (4,5). Due to their increasing prevalence and mortality, CRE, CRPA, and CRAB are at the top of the report, in which the World Health Organization (WHO) lists the factors that threaten human health (6,7).
The distribution of carbapenemase subtypes contributing to resistance varies across countries. In many Mediterranean countries, including Türkiye, infections caused by Enterobacterales producing OXA-48-type carbapenemase, classified as class D under the Ambler classification, have become increasingly prevalent. The first recognition that different OXA-48-producing Klebsiella pneumoniae clones could cause a nosocomial outbreak occurred in Istanbul in 2006 (8).
No novel antibiotics have been developed in the last 30 years; however, newly developed agents within existing antibiotic classes have been introduced for resistant infections. One of these, ceftazidime-avibactam (CAZ-AVI), was approved by the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) in 2015. CAZ-AVI combines ceftazidime, a third-generation cephalosporin with antipseudomonal activity, and avibactam, a non–β-lactam β-lactamase (1). This combination is effective against β-lactamases such as OXA-48 and K. pneumoniae carbapenemase (KPC) (9). For infections caused by OXA-48-producing microorganisms, which are the dominant carbapenemase type in certain regions of Europe, particularly Türkiye, CAZ-AVI is the first-line treatment recommended in guidelines.
Ceftazidime-avibactam was introduced in Türkiye on April 28, 2021, for the treatment of infections caused by resistant Gram-negative bacteria. Its use, however, is regulated by the Turkish Ministry of Health’s Health Implementation Communiqué, which restricts its administration to patients in intensive care units (ICUs). Its use in non-ICU patients is highly limited, and empirical therapy is not permitted, significantly constraining its application in routine clinical practice (10).
This study aimed to determine the indications for CAZ-AVI use, evaluate its clinical and microbiological efficacy, and assess side effects based on real-world experience in Türkiye. Additionally, it sought to identify the factors influencing mortality in infections caused by resistant Gram-negative bacteria.
Materials and Methods
Study Design
This retrospective cohort study was coordinated by the Department of Infectious Diseases and Clinical Microbiology, Selçuk University School of Medicine (Konya, Türkiye), and involved 22 specialists from 16 centers located in different geographical regions. Patients with carbapenem-resistant and CAZ-AVI-susceptible Gram-negative bacterial infections who were followed at the participating sites between April 2021 and September 2023 and received CAZ-AVI as part of their treatment were retrospectively reviewed.
Patient Characteristics
Patients meeting the inclusion criteria were enrolled in the analysis.
Inclusion criteria:
- Aged 18 years and over,
- Growth of carbapenem-resistant Gram-negative bacteria in any clinical culture,
- The identified microorganism being susceptible to CAZ-AVI,
- Use of CAZ-AVI for more than 48 hours in the treatment of the causative agent,
- Patient data not included in any other national or international multicenter study.
Exclusion criteria:
- Pregnant patients,
- Patients with missing data,
- Presence of a concomitant infection with another pathogen.
The study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the Non-Interventional Ethics Committee of Selçuk University School of Medicine (Approval No: 2020/16-E.584849).
Data Collection
All patients who received CAZ-AVI for any indication under the supervision of 22 infectious diseases and clinical microbiology specialists at 16 participating centers between April 2021 and September 2023 were included in the data collection process. Patient data were obtained from each center’s electronic medical records and entered into standardized study forms prepared for this research.
The study forms included demographic data, Sequential Organ Failure Assessment (SOFA), and Acute Physiology and Chronic Health Evaluation II (APACHE II) scores at baseline, comorbidity status, and indications for CAZ-AVI use (e.g., pneumonia, bacteremia, urinary tract infection [UTI], intra-abdominal infection). Culture results and identified pathogens (Escherichia coli, P. aeruginosa, K. pneumoniae, etc.), CAZ-AVI dosing, treatment method (monotherapy or combination therapy), duration of therapy, and observed side effects were also recorded.
Laboratory parameters, including white blood cell (WBC, ×109/L), C-reactive protein (CRP, mg/L), and procalcitonin (PCT, µg/L), were recorded at baseline (day 0), day 3, and day 7 of treatment. Microbiological eradication and mortality rates were documented accordingly.
Treatment Selection and Responses
A specific protocol was not applied for treatment selection, administration route, or treatment duration. The diagnosis of infection and the choice of therapy were determined by the attending infectious diseases specialist at each participating center, without additional predefined criteria for patient selection. A standard CAZ-AVI dose of 2.5 g every 8 hours was administered to all patients with normal glomerular filtration rates (GFRs). Dosages were adjusted appropriately in patients whose GFR values changed. Patients were followed in the hospital until death or discharge.
Treatment response was assessed based on all-cause mortality at days 7, 14, and 28. Microbiological eradication was defined as the absence of growth of the initial pathogen in follow-up cultures obtained at least 72 hours after treatment initiation.
Microbiological Analysis
Ceftazidime-avibactam susceptibility testing was performed using the disk diffusion method in the local laboratories of the participating centers. According to the recommendations of the European Committee on Antimicrobial Susceptibility Testing (EUCAST), in vitro antibiotic susceptibilities were determined using a 10/4 µg CAZ-AVI disk. Isolates were considered susceptible if ≥13mm and resistant if <13 mm for Enterobacterales, and susceptible if ≥17 mm and resistant if <17 mm for P. aeruginosa (11).
Statistical Analysis
Data were analyzed using IBM SPSS Statistics version 23 (IBM Corp., Armonk, NY, USA). The Pearson chi-square test was used for categorical variables. The normality of data distribution was assessed using the Kolmogorov-Smirnov and Shapiro-Wilk tests. The Friedman test was used to compare non-normally distributed parameters across three time points, and the Dunn test was applied for multiple comparisons. For normally distributed paired data, independent sample t-tests were used.
Binary logistic regression analysis was performed to identify the factors associated with mortality at days 7, 14, and 28. Receiver operating characteristic (ROC) curve analysis was used to determine the threshold values of parameters predictive of mortality at these time points. For each cut-off value, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated along with 95% confidence intervals (CIs). The area under the ROC curve (AUC) was also reported.
Categorical variables were expressed as frequencies (percentages), and continuous variables as means ± standard deviations (SDs) or medians (minimum–maximum), as appropriate. P-value < 0.05 was considered statistically significant.
Results
A total of 1245 patients meeting the study criteria were included in the analysis. Of these, 778 (62.5%) were male and 467 (37.5%) were female, with a median age of 67 years (range, 18–97). The most common indication for CAZ-AVI use was hospital-acquired pneumonia (47.8%), followed by bloodstream infection (19.3%). The predominant causative pathogen was K. pnemoniae (81.3%), followed by P. aeruginosa (12.4%). Bacteremia was detected in 34.8% of patients with UTI, 21.6% with pneumonia, and 12.5% with intra-abdominal infection.
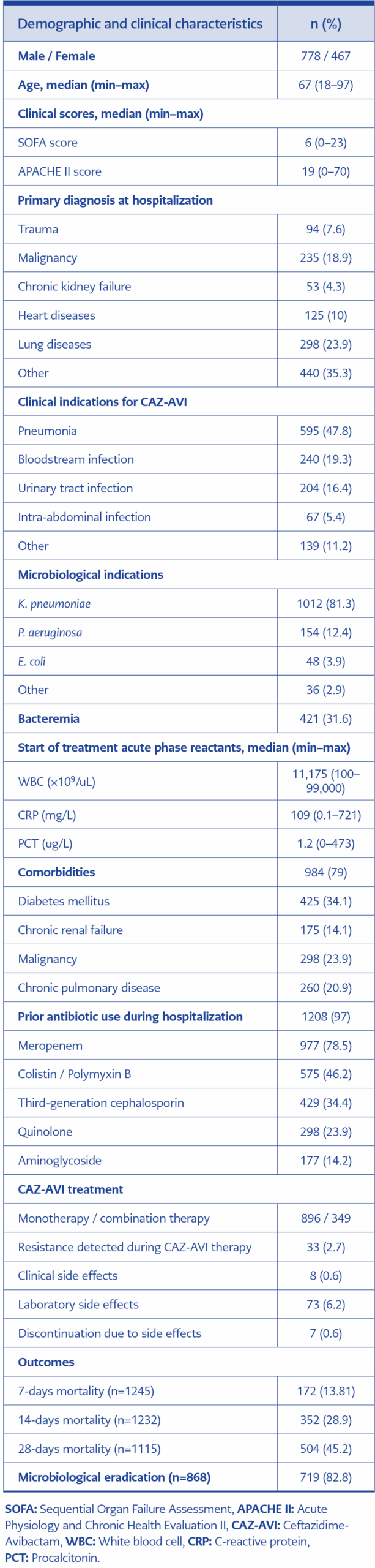
The mean duration of CAZ-AVI therapy was 11.3 ±4.8 days. It was administered as monotherapy in 80% of patients, and in 20% it was combined with another antibiotic at the treating physician’s discretion to enhance Gram-negative coverage. The demographic and clinical characteristics of the patients are presented in Table 1.
Clinical side effects were observed in 8 (0.64%) patients, and abnormal laboratory findings were reported in 73 (5.86%) patients. Clinical side effects included mild allergic reactions without anaphylaxis in 5 (0.40%) patients, gastrointestinal irritation in one, and headache in two. Seven of the eight patients who developed clinical side effects were receiving CAZ-AVI monotherapy. No treatment discontinuation occurred due to clinical side effects.
Among the 73 patients who developed abnormal laboratory findings, 43 (59%) were in the monotherapy group and 30 (41%) were in the combination therapy group. Laboratory abnormalities were significantly more frequent in patients receiving combination therapy (p=0.035). Treatment discontinuation due to laboratory abnormalities was required in 7 of 73 patients (9%) (Table 2).
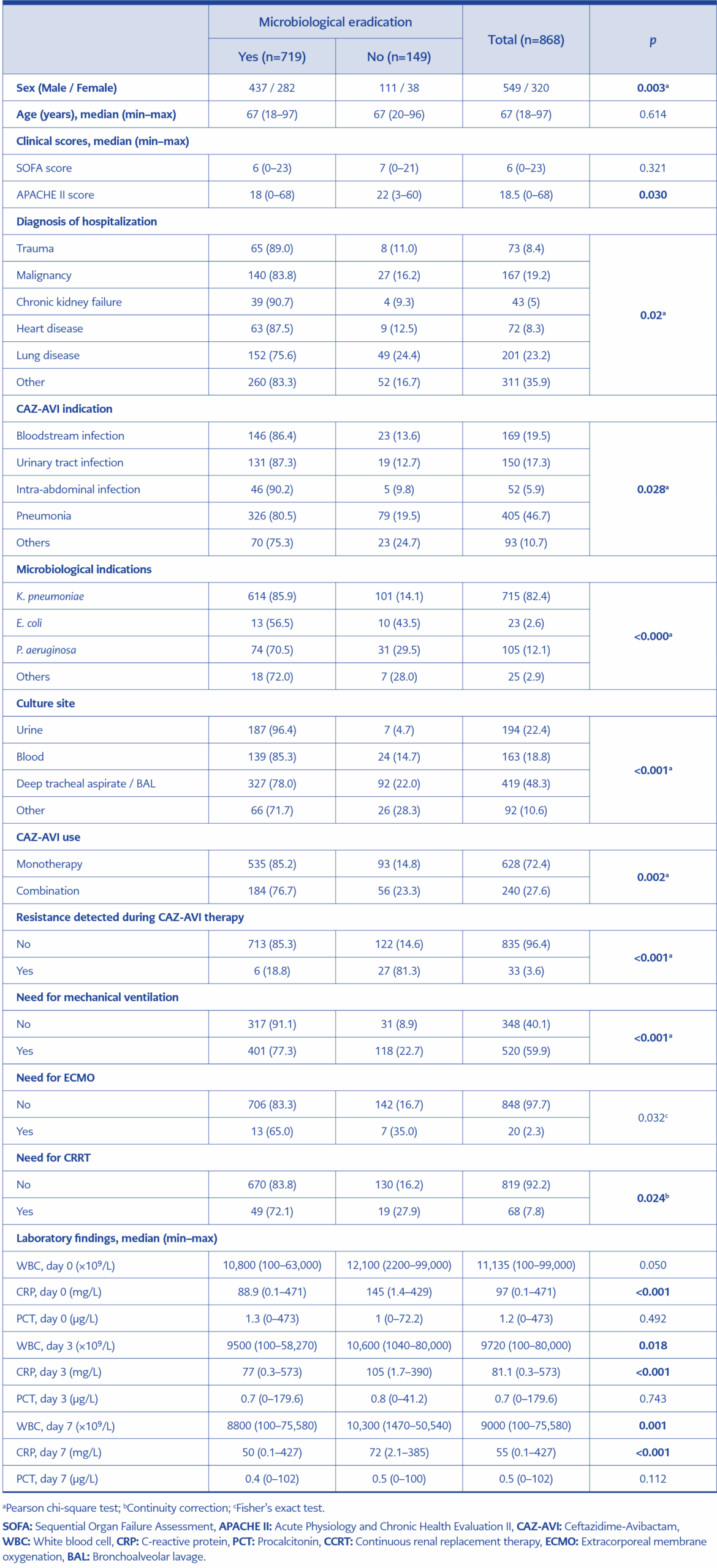
The overall microbiological cure rate was 82.8%. Infections caused by K. pneumoniae showed a cure rate of 85.9%. A statistically significant difference in microbiological cure rates was observed according to the causative microorganism (p<0.001). All variables affecting microbiological cure are summarized in Table 2.
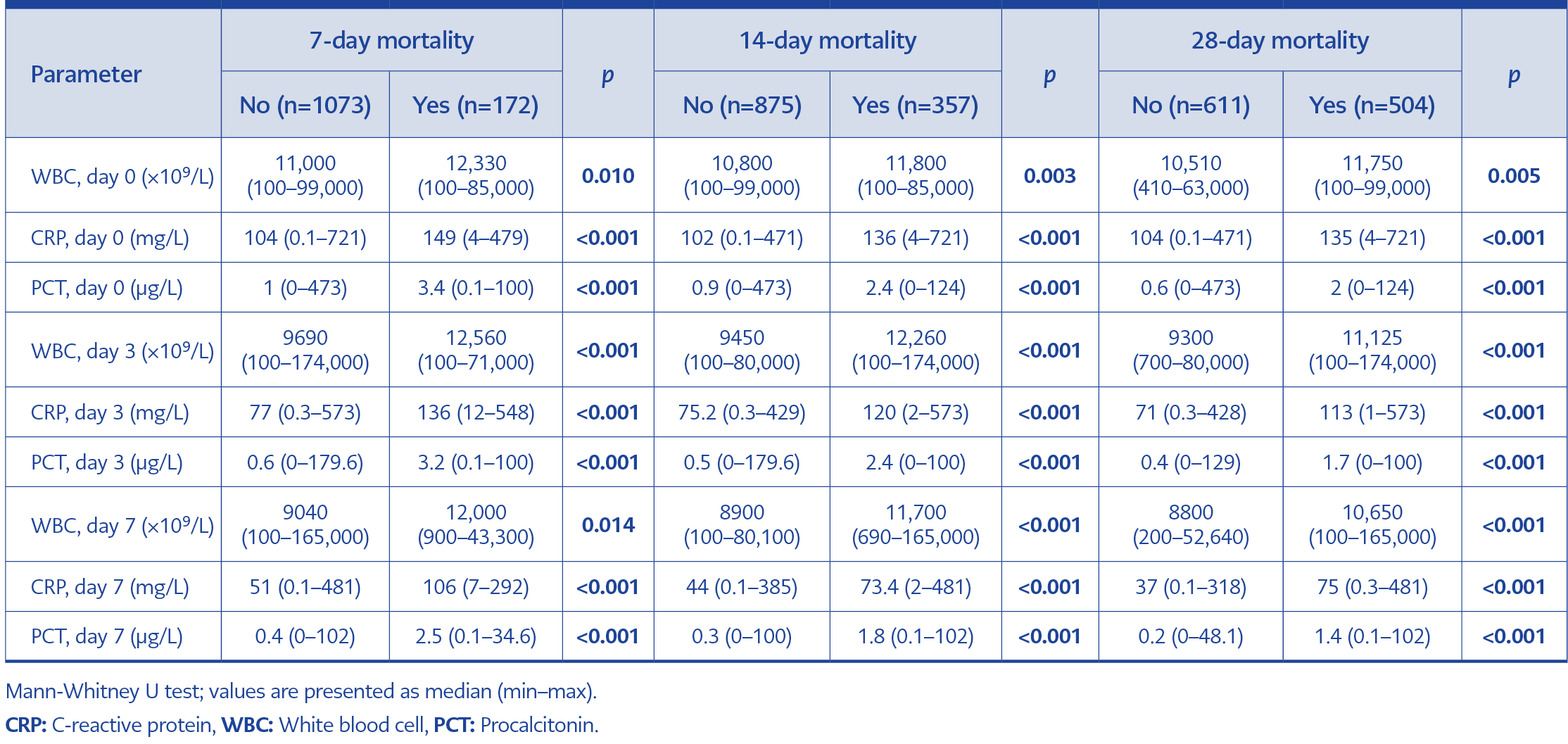
Table 4. WBC, CRP and PCT values of the patients at the beginning of treatment and on the 3rd and 7th days.
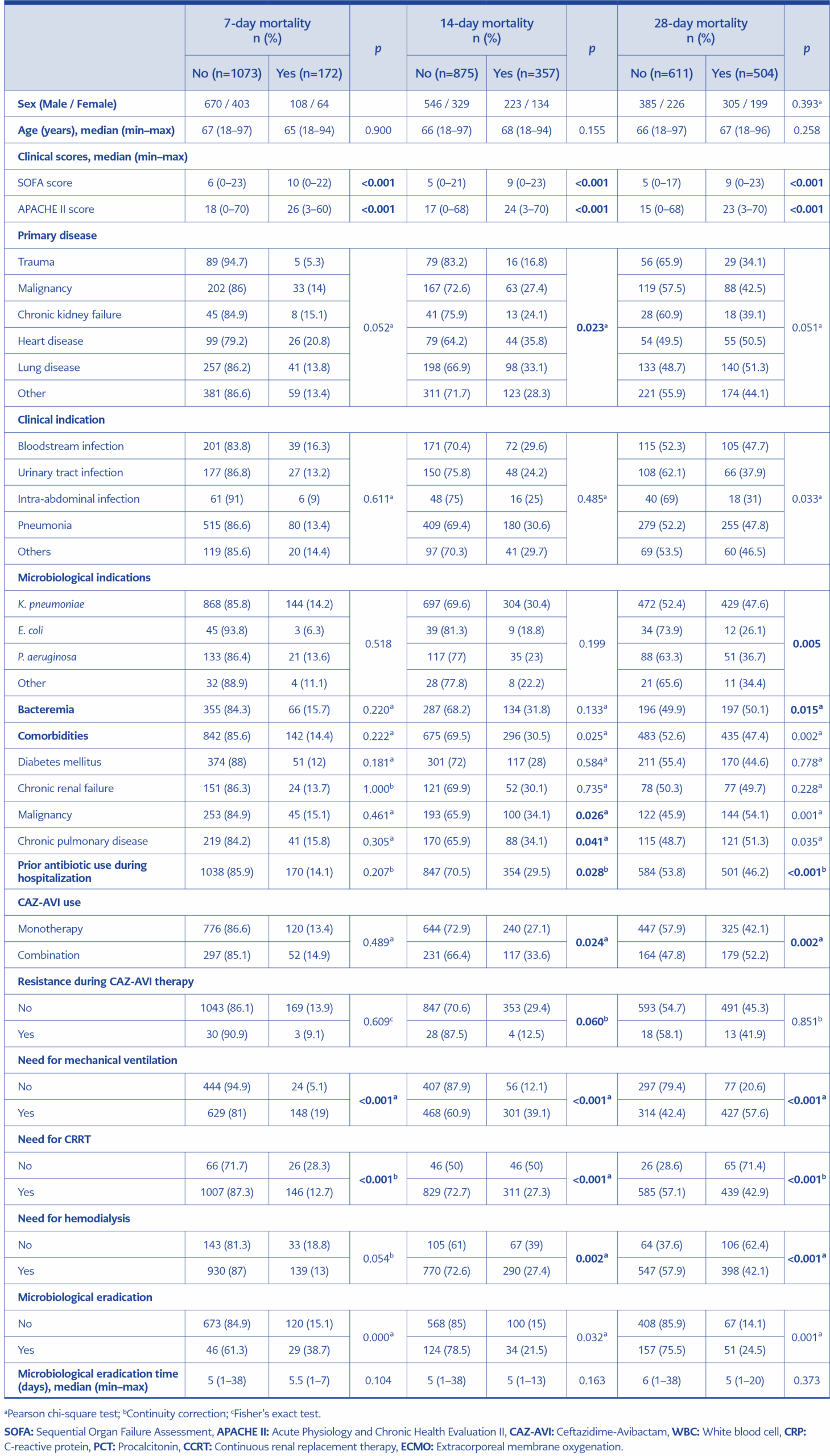
The 7-day all-cause mortality rate was 13.8%, the 14-day mortality rate was 28.9%, and the 28-day mortality rate was 45.2%. Baseline SOFA and APACHE II scores were significantly higher in the patients who died (p<0.001). An all analysis of the factors associated with 7-, 14-, and 28-day mortality is presented in Table 3, and pretreatment and follow-up laboratory parameters are shown in Table 4.
Binary logistic regression analysis identified mechanical ventilation and continuous renal replacement therapy (CRRT) as independent risk factors for mortality for all three time points (days 7, 14, and 28). For mechanical ventilation, the odds ratios (ORs) and 95% CIs were as follows:
Day 7: OR 3.038; 95% CI 1.809–5.102; p<0.001
Day 14: OR 4.366; 95% CI 3.04–6.271; p<0.001
Day 28: OR 3.642; 95% CI 2.481–5.345; p<0.001
For CRRT, the results were as follows:
Day 7: OR 1.877; 95% CI 1.071–3.29; p=0.028
Day 14: OR 2.114; 95% CI 1.219–3.667; p=0.008
Day 28: OR 1.811; 95% CI 1.107–2.964; p=0.018
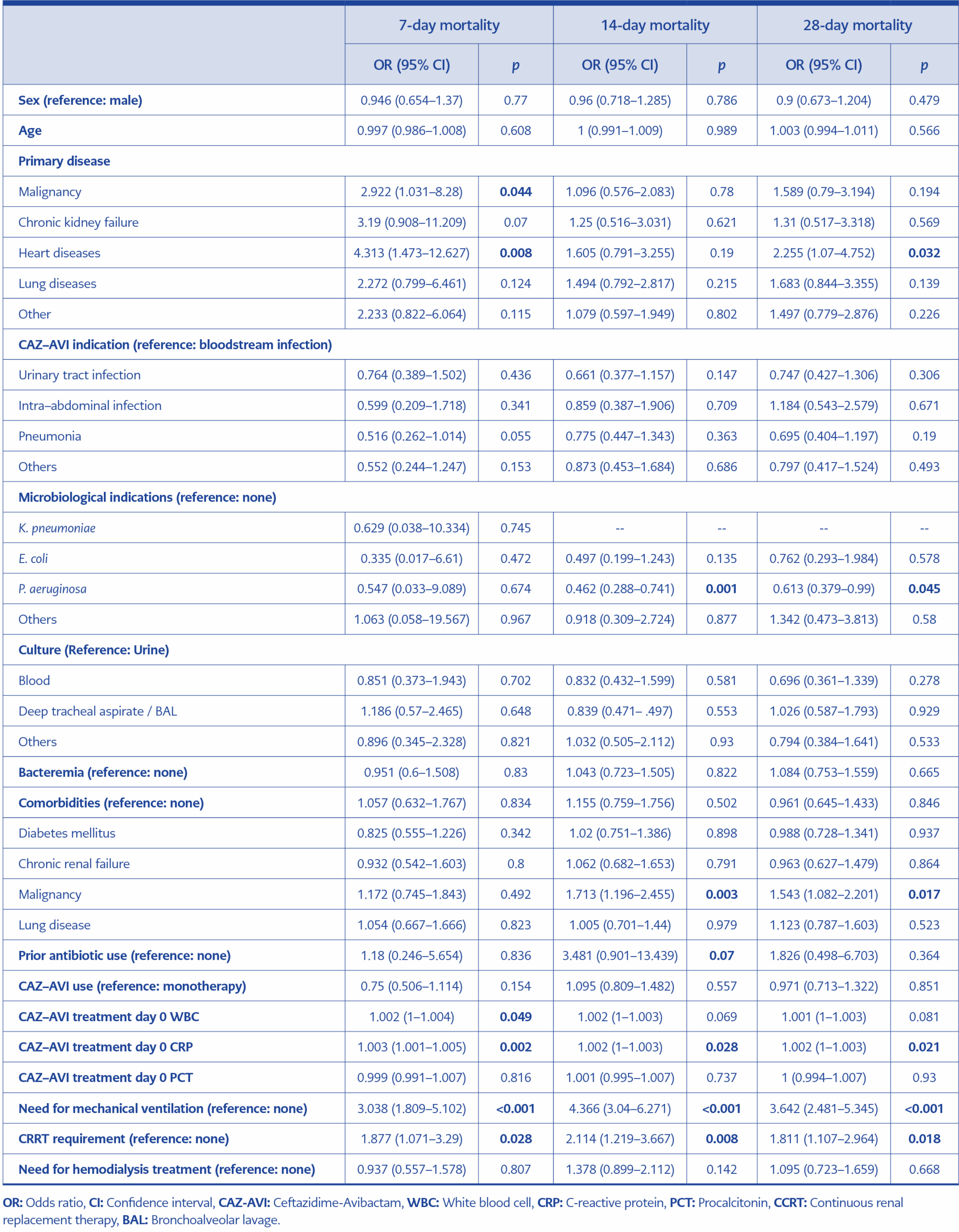
Table 5. Examination of factors affecting 7, 14 and 28-day mortality using binary logistic regression analysis.
All variables identified as mortality risk factors in the binary logistic regression analysis are summarized in Table 5.
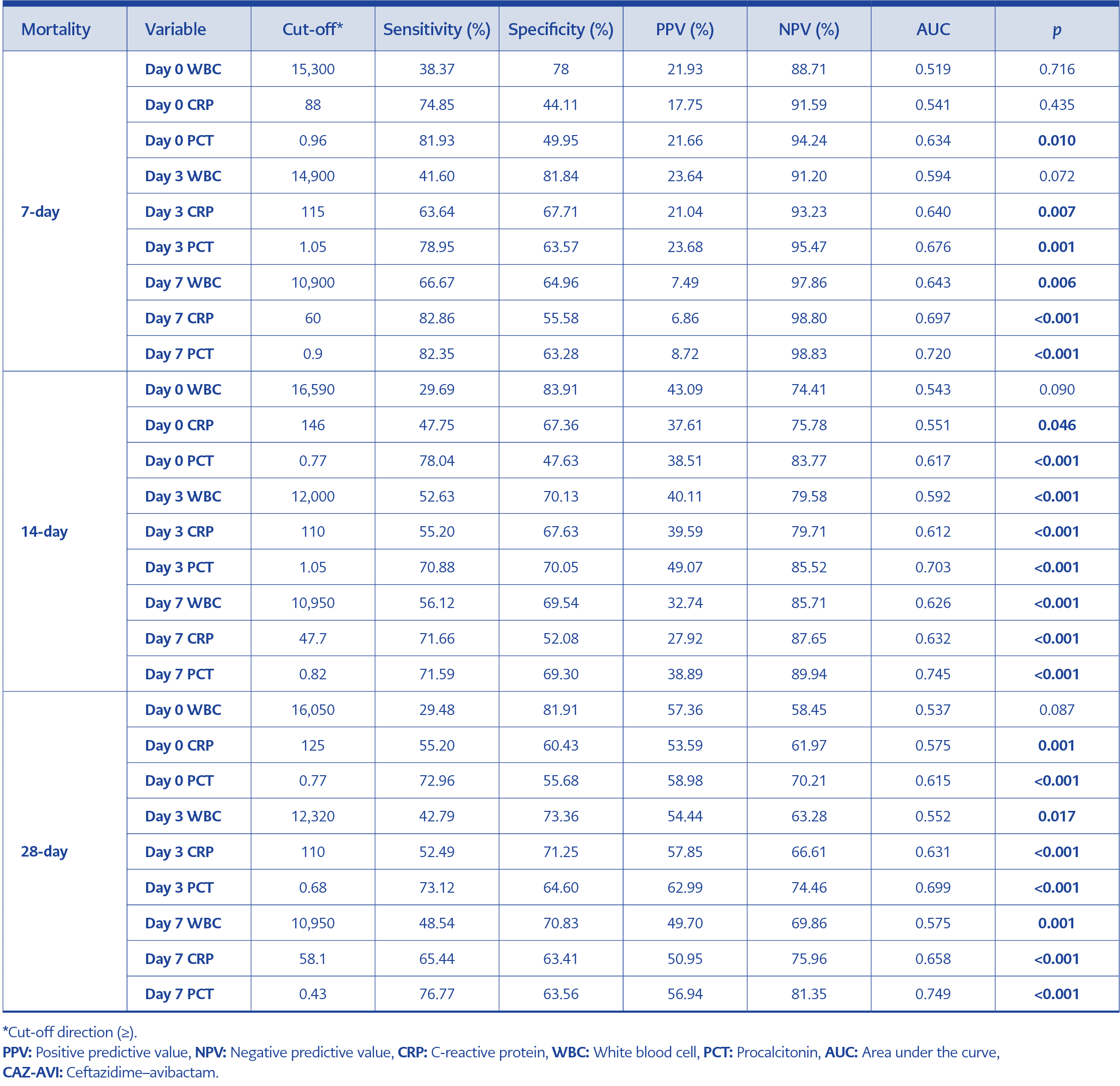
Table 6. Receiver operating characteristic (ROC) analysis results for 7-, 14-, and 28-day mortality according to CAZ-AVI treatment.
The Area Under the Curve (AUC) value for PCT at baseline (day 0) in predicting 7-day mortality was 0.634, which was statistically significant (p=.01). Taking the threshold value as 0.96 at day 0, the sensitivity turned out to be 81.93%, specificity 49.95%, PPV 21.66%, and NPV 94.24%. The AUC value for CRP at day 3 in predicting 7-day mortality was 0.64, and the AUC value at day 7 was 0.697, which were statistically significant (p=0.007 and p=0.001, respectively). With a threshold value of 115 at day 3 of CAZ-AVI therapy, the sensitivity was 63.64%, specificity 67.71%, PPV 21.04%, and NPV 93.23%. The AUC value for WBC at day 7 of the therapy was 0.643 (p=0.006). With a threshold value of 10,900 at day 7, the sensitivity was 66.67%, specificity 64.96%, PPV 7.49%, and NPV 97.86%. All ROC analysis results of PCT, CRP, and WBC values, together with their threshold values, PPV, and NPV for predicting 7-, 14-, and 28-day mortalities, are summarized in Table 6.
Discussion
Türkiye is considered an OXA-48–dominant region according to several reports; however, the distribution of carbapenemase types is changing rapidly. A recent study demonstrated OXA-48 positivity in 52.2% and KPC positivity in 16.1% of E. coli and K. pneumoniae isolates (12). For this reason, CAZ-AVI plays an important role in the treatment of Gram-negative infections in Türkiye. Our study is the most comprehensive multicenter real-world analysis in an OXA-48–dominant region and, to our knowledge, the first to investigate the predictive value of WBC, CRP, and PCT thresholds for mortality.
Previous studies and reviews have shown that CAZ-AVI is most commonly used against CRE infections and, less frequently, against P. aeruginosa (13-16). A systematic review of 1926 patients reported that CRE (n=1718) and multidrug-resistant P. aeruginosa (n=150) were the most common pathogens treated with CAZ-AVI (15). The distribution of causative pathogens in our series was similar to that reported in the literature.
In the review by Soriano et al. (15), which included 73 articles involving 1926 patients who received CAZ-AVI therapy between 2015 and 2021, the most common indications were pneumonia and bacteremia. Many other studies have reported the use of CAZ-AVI for various infections, and, similar to our study, pneumonia was the most frequent indication (3, 17-20).
The superiority of the combination therapy with CAZ-AVI over monotherapy has not been demonstrated; similar efficacy rates have been reported (21). Tumbarello et al. (22), in a review of 577 patients with KPC-producing K. pneumoniae infections, found no significant difference in clinical outcomes between CAZ-AVI monotherapy and combination therapy. Similarly, Onorato et al. (23) reported in their meta-analysis that mortality rates were higher with combination therapy, as was also the case in our study. This may be explained by the fact that patients receiving combination therapy generally had more severe baseline conditions than those receiving monotherapy. Additionally, the potential adverse effects associated with the second drug could have negatively influenced outcomes. Overall, our findings support the use of CAZ-AVI monotherapy for both efficacy and safety, consistent with previous reports.
In the REPRISE Phase 3 trial, in which CAZ-AVI was compared with other treatment options for complicated UTIs and intra-abdominal infections caused by Enterobacteriaceae and P. aeruginosa in 53 hospitals across 16 countries, clinical side effects, mostly gastrointestinal, were reported in 51 of the 164 patients receiving CAZ-AVI, and none required discontinuation (24). Jorgensen et al. (3) reported adverse events in 17 (8.4%) of 203 patients, including 10 cases of acute kidney injury. The overall incidence of CAZ-AVI-related adverse events is quite low in studies, and most did not require treatment discontinuation (3,22,25). Our study confirms these findings and further demonstrates that CAZ-AVI is a well-tolerated antibiotic.
Carbapenem-resistant Gram-negative infections are associated with high mortality, with rates of up to 70% reported in some series (26). In real-world CAZ-AVI experiences, all-cause mortality has ranged between 8% and 40% (13,14,25,27). In our study, the 28-day mortality rate was 45.2%, which is high but within the upper range of previously published data. Several factors may explain this finding: most patients were critically ill, with high baseline APACHE II (median 19) and SOFA (median 6) scores; a substantial proportion were in the ICU and required mechanical ventilation; and many had severe comorbidities. These determinants are well established as independent risk factors for mortality (3,14,16).
The microbiological eradication rate in our study (82.3%) was within the previously reported range of 68–90% (13,16,20,24). Notably, treatment failure was most frequent in patients with pneumonia (19.5%), consistent with previous reports identifying pneumonia as the infection type with the highest risk of therapeutic failure (28-30).
In our study, the baseline serum concentrations of PCT, CRP, and WBC were significantly lower in survivors than in non-survivors; however, only CRP remained an independent determinant in multivariate analysis. Similar to our findings, studies conducted in intensive care populations have shown higher baseline PCT, CRP, and WBC levels in non-survivors (31,32). Nevertheless, their predictive power for mortality remains uncertain, and the literature is inconsistent. A study investigating septic shock patients reported that baseline CRP and PCT values alone had limited value in predicting 28-day mortality (33). Similarly, another study found that baseline CRP and PCT levels were not associated with mortality, but low CRP and PCT clearance during treatment were directly associated with treatment failure (34). In our analysis, serum CRP, PCT, and WBC levels were significantly higher in non-survivors, and ROC analysis demonstrated their predictive value for 7-, 14-, and 28-day mortality. Although CRP emerged as the only independent predictor in multivariate analysis, our study provides novel insight by identifying clinically relevant thresholds for these biomarkers. To our knowledge, no prior study has reported such findings.
Our study has several limitations. Molecular resistance mechanisms were not investigated, and polymicrobial infections could not be fully differentiated. Data regarding the specific combination therapies were incomplete. Furthermore, CAZ-AVI was not evaluated as empirical therapy, as national regulations restrict its use to documented infections with confirmed susceptibility. Finally, although the retrospective design reflects real-world practice, it limited access to certain clinical data and may introduce reporting bias.
In conclusion, this is the largest multicenter real-world study of CAZ-AVI conducted in an OXA-48–dominant country. Clinical and microbiological outcomes were evaluated across a broad range of infection types, and risk factors for mortality were analyzed together with biomarker thresholds. We believe these findings provide valuable guidance for clinicians managing carbapenem-resistant Gram-negative infections in regions with similar resistance patterns.