Introduction
Vaccination is a key component of preventive health services to combat infectious diseases. While pediatric vaccination programs are well-established in the national immunization programs (NIPs) of many countries, leading to substantial global progress, adult vaccination programs often receive less attention. With advancing age and the presence of chronic comorbid conditions, vaccine-preventable diseases (VPDs) such as influenza, pneumococcal disease, herpes zoster, and respiratory syncytial virus (RSV) pose a higher risk of infection and significantly contribute to healthcare costs, morbidity, and mortality (1-2). In the United States alone, VPDs are estimated to cause 40,000–50,000 adult deaths annually, with associated treatment costs nearing 27 billion USD (3-6). As life expectancy continues to rise, the burden of VPDs is expected to grow further (7,8). Pneumococcal pneumonia remains one of the most significant VPDs in adults and accounts for a substantial proportion of VPD-related morbidity and mortality (9).
Adult vaccination programs provide important clinical benefits by reducing mortality and morbidity. They are highly cost-effective and can deliver net cost savings for healthcare systems (7). Despite these advantages, global adult vaccination rates remain suboptimal (10). Strengthening coverage and improving the effectiveness of adult vaccination, particularly among older adults, is essential to reducing the burden of VPDs (8,10). Although childhood NIPs reduce pneumococcal disease in adults through indirect (herd) protection, their impact is limited because children are not the only source of transmission. Given this context, we aimed to review current knowledge regarding the burden of pneumococcal disease in adults and the role of pneumococcal vaccines in prevention, incorporating available data from Türkiye.
Invasive Pneumococcal Disease
Streptococcus pneumoniae (pneumococcus) causes a spectrum of non-invasive diseases (sinusitis, otitis media, and non-bacteremic pneumonia) and invasive diseases (bacteremic pneumonia, sepsis, and meningitis) (11).
Invasive pneumococcal disease (IPD) refers to an infection in which the bacterium infiltrates a sterile site, such as blood, cerebrospinal fluid, pleural fluid, joint fluid, or pericardial fluid. Invasive pneumococcal disease presents with a more severe clinical course compared with non-invasive pneumococcal disease (NIPD) (11). Although pneumococcal pneumonia, primarily classified as NIPD, occurs more frequently than IPD (12), robust data on community-acquired NIPD pneumonia in adults aged ≥65 years remain limited. A systematic review of U.S. studies published between 1995 and 2019 estimated pneumonia hospitalization rates between 1% and 3% (847–3365 per 100,000 population), with NIPD and IPD incidence reported at 105 and 24 cases per 100,000 population, respectively (13,14).
During 2020 and early 2021, the global incidence of IPD decreased substantially due to social distancing measures implemented during the COVID-19 pandemic. However, rates returned to pre-pandemic levels —or exceeded them— later in 2021 (15). The burden of IPD is primarily driven by bacteremic pneumonia, pneumococcal meningitis, and primary bacteremia. In a U.S. epidemiological study (1995–1998), involving ~16,000 IPD cases, 53% presented with pneumonia, 40% with primary bacteremia, and 4.5% with meningitis (16,17).
The incidence of IPD is highly age-dependent, with 38% of cases occurring in children <2 years and 54% in adults >50 years (18). Reported all-age IPD incidence ranges from 11–27 per 100,000 population in Europe and 15–49 per 100,000 in North America, while some Asian countries report higher rates —for instance, Taiwan has reported annual incidences up to 216 per 100,000 (19-24). Invasive pneumococcal disease also carries substantial mortality, with case-fatality rates reported up to 35% among adults ≥65 years (25).
A 2021 systematic review by Navarro-Torné et al. (26) estimated pooled IPD incidences of 15.08 per 100,000 population (95% confidence interval [CI] 11.01–20.65) in Spain and 2.56 per 100,000 (95% CI 1.54–4.24) in Italy. The study also showed a significant decrease in IPD caused by 7-valent pneumococcal conjugate vaccine (PCV7) serotypes —from 19.10 to 5.50 cases per 100,000— among populations aged ≥60 or ≥65 years. Additionally, a global burden of disease study on lower respiratory tract infections (LRTIs) estimated 2,377,697 deaths globally (2,145,584–2,512,809), including 1,080,958 deaths (943,749–1,170,638) among adults >70 years (27).
A 12-year study from Croatia (2010–2022) reported annual IPD incidences ranging from 0.6 to 4.1 per 100,000, with 47.6% of cases occurring in adults ≥65 years and 79.4% in those ≥ 50 years (28). In Türkiye, data on the prevalence of IPD in the adult population remain limited.
Non-Invasive Pneumococcal Disease
Non-Invasive pneumococcal disease (NIPD) is approximately five times more prevalent than IPD (29). Although NIPD includes sinusitis, acute otitis media, and community-acquired pneumonia (CAP), this review primarily focuses on pneumococcal CAP given its substantial impact in adults. Microbiological diagnosis is typically established in about 20% of CAP cases (30). S. pneumoniae and Haemophilus influenzae are the most commonly identified bacterial pathogens, while rhinovirus and influenza are predominant causative agents in viral cases. A European review reported S. pneumoniae as the most common pathogen, accounting for 35% of cases overall, with rates varying between 12% and 68% globally (18). Although national data from Türkiye remain limited, the isolation rate of S. pneumoniae has been reported between 14.7% and 25% (31).
Due to the challenges of confirming non-bacteremic pneumococcal CAP, its true incidence remains uncertain. The estimated annual incidence of CAP across European countries ranges from 0.068% to 7% (32). A retrospective, population-based cohort study (33) conducted in Spain between 2017 and 2018 showed that the incidence and case-fatality rates of pneumococcal CAP increase significantly with age. Additional risk factors for pneumococcal CAP include immunocompromised status, a history of prior IPD or pneumonia, and the presence of multiple coexisting comorbidities (i.e., two or more underlying conditions) (33).
More than 100 pneumococcal capsular serotypes have been identified, with each exhibiting different tendencies toward asymptomatic colonization and the development of non-invasive or invasive disease (34).
Available Pneumococcal Vaccines for Use in Adults and Current Recommendations
Two types of pneumococcal vaccines are available for adults: pneumococcal polysaccharide vaccine (PPSV) and PCV. Pneumococcal polysaccharide vaccine induces a T-cell-independent B-cell response, resulting in short-lived immunity without an anamnestic response, necessitating revaccination (35,36). In contrast, PCVs consist of capsular polysaccharides covalently linked to an immunogenic carrier protein, eliciting a T-cell-dependent immune response. This leads to long-term immunologic memory and an anamnestic response. Additionally, PCVs stimulate mucosal immunity, reducing nasopharyngeal colonization and indirectly protecting unvaccinated individuals (37,38).
Including an excessive number of serotypes may cause immune interference, potentially diminishing vaccine effectiveness. Increasing valency also increases complexity and costs in production. Moreover, pneumococci do not exhibit broad cross-protection among serotypes, unlike some other pathogens. Therefore, serotype selection prioritizes the most prevalent and most pathogenic in the population (39-41).
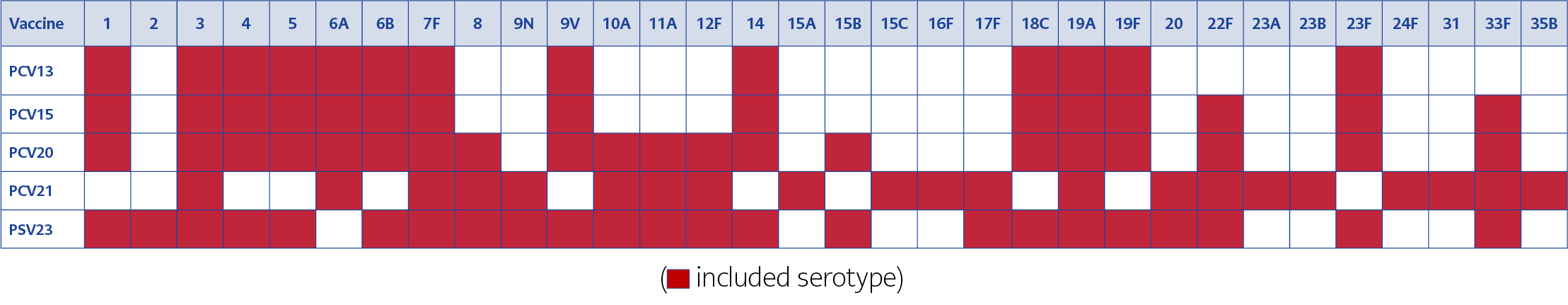
The 13-valent PCV (PCV13) and 23-valent PPSV (PPSV23) have been used worldwide in adults for many years. National immunization program implementation in various countries has reduced vaccine-serotype pneumococcal disease, even though non-vaccine serotypes have become more prevalent (42). As diseases caused by non-PCV13 and non-PPSV23 serotypes emerged (41), the need for a higher-valency conjugate vaccine became evident, leading to the development of 15-valent and 20-valent PCVs (PCV15 and PCV20). The 21-valent PCV (PCV21) was licensed by the U.S. Food and Drug Administration (FDA) in June 2024 for use in individuals aged ≥18 years (43,44). The pneumococcal vaccines currently available for adults in Türkiye are listed in Table 1 (45).
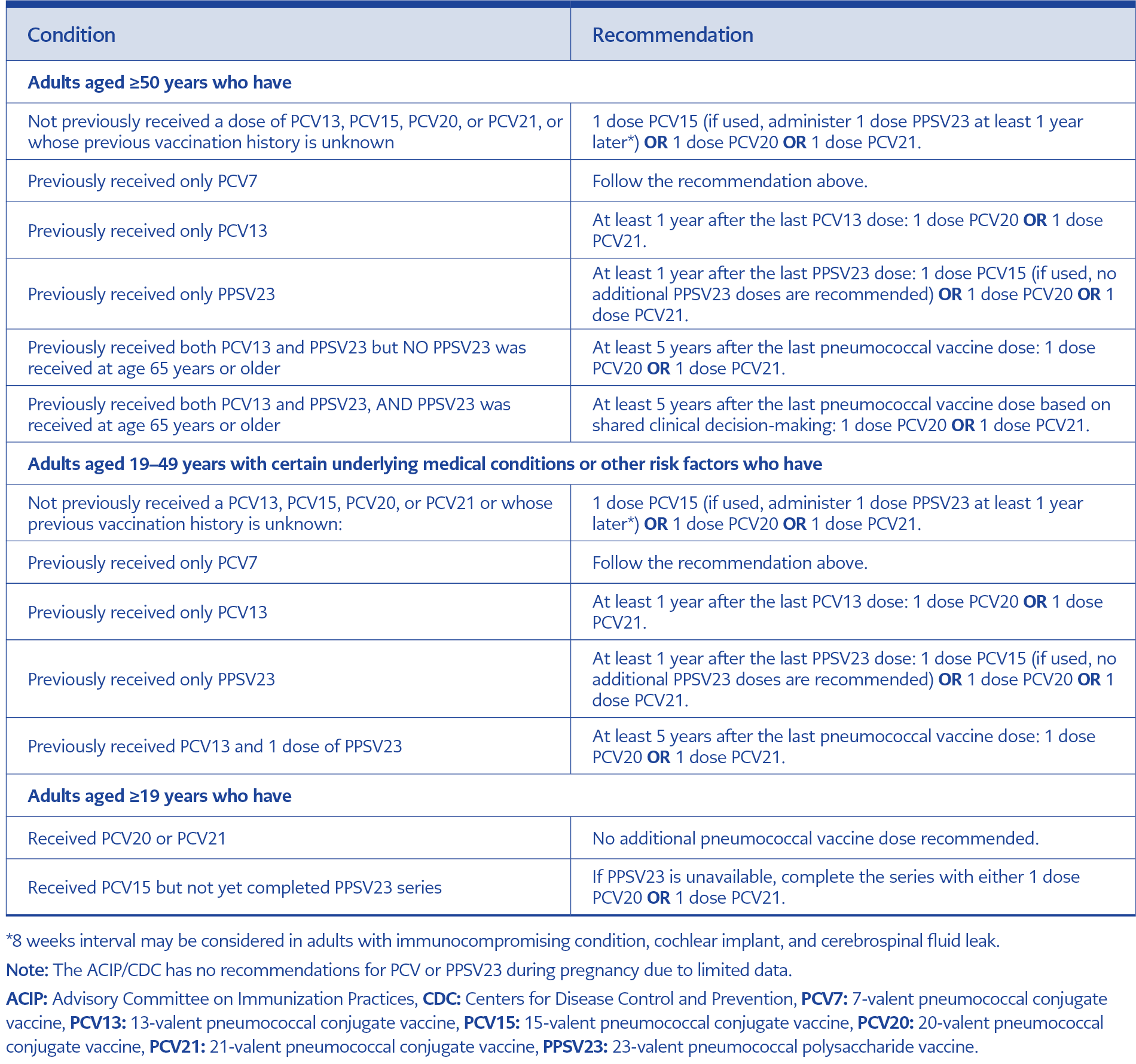
The Advisory Committee on Immunization Practices (ACIP) and the U.S. Centers for Disease Control and Prevention (CDC) updated their recommendations for the use of pneumococcal vaccines for adults in October 2024 (46). The ACIP/CDC recommends PCV for all PCV-naïve adults aged ≥50 years, as well as for adults aged 19–49 years with underlying risk factors who have not previously received a PCV or whose vaccination history is unknown (46). The 2025 Adult Immunization Schedule recommendations for pneumococcal vaccinations are summarized in Table 2.
PCV21 contains eight serotypes (15A, 15C, 16F, 23A, 23B, 24F, 31, 35B) not contained in earlier PCV formulations, in place of several previously included serotypes (e.g., 1, 4, 5, 19F) (44). The serotype composition of available pneumococcal vaccines is illustrated in Figure 1.
The Infectious Diseases and Clinical Microbiology Specialty Society of Türkiye (EKMUD) (47) and the Turkish Society of Clinical Microbiology and Infectious Diseases (KLİMİK) (48) recommend PCV vaccines (PCV13, PCV15, PCV20, or PCV21, depending on availability) for older adults and for adults with comorbidities. Since 2016, PCV13 has been provided at no cost in Türkiye to adults aged ≥65 and other at-risk adults through healthcare institutions. PPSV23 is also covered when prescribed for risk groups as defined in the Healthcare Implementation Communiqué (Sağlık Uygulama Tebliği, SUT) (49,50).
The Ministry of Health has identified the following risk groups for whom pneumococcal vaccination is recommended (51): individuals with chronic heart disease (especially cyanotic congenital heart disease and heart failure), chronic pulmonary disease (including asthma), chronic kidney disease and nephrotic syndrome, chronic liver disease, diabetes mellitus, cerebrospinal fluid leakage, cochlear implants, sickle cell anemia and other hemoglobinopathies, functional or anatomic asplenia, HIV infection, immunosuppressive therapy (e.g., radiation therapy, immunosuppressive therapy, and congenital or acquired immunodeficiency), Hodgkin’s disease, malignant diseases (including lymphoma, leukemia, and multiple myeloma), solid organ transplantation, hematopoietic stem cell transplantation, and alcoholism.
Effectiveness of Pneumococcal Vaccines
The impact of PCVs is considered a major public health achievement. Nearly 100 million adults worldwide received PCV13 over the past decade, potentially preventing 662,000 pneumococcal cases and 4.1 million IPD cases through indirect protection (52). However, accurately measuring the full benefit of the vaccine remains challenging. Surveillance systems typically capture only a subset of pneumococcal cases and vaccine-preventable deaths. Variability in vaccination coverage, dosing schedules, incomplete vaccination, indirect effects, and sero-epidemiology further complicate assessment. As a result, published estimates may substantially underestimate the true impact of PCVs; it has been suggested that the number of pneumococcal diseases prevented over the last decade may be up to three times higher than currently reported (52).
Pneumococcal infection is associated with increased morbidity and mortality among adults with cardiovascular disease. Several studies have demonstrated the potential benefits of pneumococcal vaccines in reducing the risk of cardiovascular events (53). A meta-analysis of 15 studies including 347,444 adults (111,784 vaccinated and 235,660 unvaccinated) found that pneumococcal vaccination was associated with reduced risk of myocardial infarction (hazard ratio [HR]=0.73; 95% CI 0.56–0.96, p=0.02) and all-cause mortality (HR=0.76; 95% CI 0.66 to 0.87, p<0.001) (54). In adults with diabetes, pneumococcal vaccination has also been associated with decreased risk of hospitalization or death, with adjusted HRs and ORs ranging from 0.76 to 0.97 across studies (55). Additional studies demonstrate protective effects of pneumococcal vaccines against CAP, IPD, and acute exacerbations of chronic obstructive pulmonary disease (COPD) (56).
Early real-world evidence from the United States shows that PCV20 provides significant protection against all IPD and all-cause pneumonia (ACP) in adults aged 65 years and older. In a large retrospective cohort study using Medicare data, PCV20 demonstrated an adjusted vaccine effectiveness of 25.6% (95% CI 19.5–31.3) against all IPD and 15.2% (95% CI 14.6–15.8) against ACP (57). It is important to note that PCV20 primarily reduces vaccine-type IPD and pneumococcal pneumonia; thus, the observed effect on IPD and ACP largely reflects its impact on vaccine-type disease rather than all etiologies of pneumonia. These protective effects were consistent across immunocompromised, chronically ill, and low-risk groups, underscoring PCV20’s public health impact in preventing pneumococcal disease among older adults (58).
Numerous studies have demonstrated that pneumococcal vaccination in adults is cost-effective (7, 59-61). A recent multinational analysis from ten countries (Australia, Brazil, France, Germany, Italy, Japan, Poland, South Africa, Thailand, and the United States of America) assessed four adult vaccines —influenza, pneumococcal, herpes zoster, and RSV— and concluded that adult vaccination programs generate substantial net monetary benefits for individuals, health systems, and society (7). Benefit-cost analyses indicate that adult vaccines can yield returns of up to 19-fold relative to investment, translating into societal net benefits of up to 4637 USD per fully vaccinated individual (7).
In Türkiye, a three-center study analyzed the direct costs of hospitalization, duration of hospital stays, and factors influencing hospitalization over a 12-month follow-up period. Among 400 vaccinated and 400 unvaccinated adults, the mean length of hospital stay was shorter in the vaccinated group (9.11 vs. 12.41). The annual per-capita hospitalization cost was 550.52 USD in the vaccinated group, compared with 703.62 USD in the unvaccinated group. Pneumococcal vaccination reduced the duration and cost of hospital stays by 41.7% and 27.8%, respectively (56,59). Furthermore, a Markov model analysis in Türkiye estimated the economic benefit of PCV13 vaccination in adults to be 207.02 USD per vaccination in 2017 (60). At a population level, PCV vaccination is estimated to prevent 200,000 CAP cases annually in Europe (62).
Despite well-established evidence of safety, efficacy, and economic value, pneumococcal infections remain a major global concern, largely due to low awareness and inadequate vaccination coverage among adults. Ongoing challenges include regional variation in disease-causing serotypes, the rise of non-vaccine serotypes, and antimicrobial resistance.
Pneumococcal Vaccine Awareness and Vaccination Rates
Even though the health and economic benefits of pneumococcal vaccines have been well demonstrated, many countries continue to report low vaccination uptake among adults, including those in high-risk groups. In a retrospective study of adults aged 19–64 years with underlying comorbidities in the United States, the pneumococcal vaccination rate among 108,159 patients was 4.1% within a 1-year follow-up period and 19.4% within a 10-year follow-up period (63). According to CDC data, the pneumococcal vaccination rate (≥1 dose of any pneumococcal vaccine) among adults aged 65–70 years is approximately 60%, which remains suboptimal (64). In Germany, the pneumococcal vaccination rate was reported to be low (about 1%) among individuals aged 16–59 years who had at least one at-risk or high-risk condition (65). A 2018 French study reported that only 4.5% of 4,045,021 at-risk adults were up to date with pneumococcal vaccination (66). Another study from Belgium found that pneumococcal vaccination coverage among at-risk adults decreased from 21% in 2017 to 18.2% in 2018, then increased to 23.6% in 2021. In 2021, coverage was highest among high-risk adults (33.8%), followed by adults aged 50–85 years with comorbidity (25.5%) and healthy adults aged 65–85 years (18.7%) (67). In China, the vaccination rate for PPSV-23 —the only pneumococcal vaccine approved for older adults— ranges from 1.23% to 42.1% across regions (68). A study from Japan evaluating 17,991 individuals aged ≥65 years reported a pneumococcal vaccination rate of 33.6% (69).
In Türkiye, although childhood vaccines included in NIP are consistently administered as part of routine medical practice, a comparable, widespread adult vaccination program is not available (70). According to the Turkish Statistical Institute, approximately 9 million adults aged ≥65 years live in Türkiye (71). The adult population younger than 65 is around 52 million, and at least 30% have one or more chronic diseases (e.g., cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes) or risk factors (e.g., obesity, physical inactivity, unhealthy lifestyle, and alcohol consumption) (72,73). These figures suggest that a substantial portion of the population should receive pneumococcal vaccination. Although the pneumococcal vaccines are provided free of charge for older adults and at-risk populations, vaccination uptake remains quite low (74). A survey of adults ≥65 years visiting family physicians (n=326) reported a vaccination rate of 4.3% (74,75). In another Turkish study of older adults (n=984), the vaccination rate was 10.9% (76). Among hemodialysis patients (n=360), the vaccination rate was 14.4%, while among diabetic patients (n=202) it was 14.7%. In individuals with COPD, the reported rate was 14.1% (77-79).
Factors Affecting Vaccination Uptake and Recommendations for Improvement
The main barriers to routine adult vaccination include prior unpleasant experiences or fear of side effects, as well as lack of trust in vaccine effectiveness (80). The most influential factor in adult vaccination is healthcare providers’ recommendations. In addition, socioeconomic status, age, education level, comorbidities, healthcare utilization, awareness of diseases and relevant vaccines, accessibility, and affordability also impact vaccination uptake (80). In China, determinants of willingness to be vaccinated include the presence of comorbidities in older adults, knowledge, beliefs, and attitudes regarding pneumococcal infections and vaccines, education level, socioeconomic status, and local policies. It has been suggested that interventions and policies —such as government funding, subsidies, inclusion of pneumococcal vaccines in health insurance programs, and proactive encouragement by healthcare workers—should be implemented as key strategies to improve vaccination rates (68).
Among older adults in Türkiye, higher vaccination rates are associated with living in urban areas, having a high school education or higher employment status, having chronic diseases, and being physically independent (76). Studies have shown that pneumococcal vaccination rates increase significantly when healthcare professionals provide information and recommend the vaccine (75,81). A survey assessing physicians’ knowledge and attitudes toward adult vaccination in Türkiye (n=435; 43.9% family physicians, 36.8% internists, and 19.3% other specialties) found that 63.4% had reviewed the NIP vaccination schedule. Physician recommendation rates were 78% for PCV13 and 48.3% for PPSV23 (82).
In a multicenter national study involving adults >18 years old who visited cardiology clinics and had never been vaccinated against pneumococcal disease (n=1808), 67.2% of patients were unaware of the pneumococcal vaccine, while 32.7% remained unvaccinated despite having prior knowledge. Additionally, 63.3% mistakenly believed that pneumococcal and influenza vaccines were the same. Television, the internet, and social media were the most common sources of information. After receiving information about the vaccine, 66% of the 1709 patients whose vaccination status was recorded during follow-up chose to be vaccinated. Vaccination uptake was significantly associated with female gender, higher education level, patient knowledge, and physician recommendation (83).
In a study conducted across three tertiary care centers, patients aged ≥65 years with risk factors for pneumococcal disease who visited the hospital were monitored for two years (n=263,302). During the study period, the hospital information management system sent pneumococcal vaccination reminders to physicians’ computers and patients’ mobile phones, consistent with guideline recommendations. Educational posters were displayed in the polyclinics, and regular seminars on the evidence of pneumococcal vaccination were held. After excluding previously vaccinated patients, 29,530 patients were evaluated. Over the study period, the annual vaccination rate reached 4.8%, representing a 74.4% increase from the previous year. Vaccination rates were higher among patients with COPD and asthma compared with adults ≥65 years without comorbidities (5.2% vs. 3.9%, p=0.002) (84).
In a study involving hemodialysis patients, individuals were informed about influenza and pneumococcal vaccines through face-to-face interviews, after which 89.7% stated that they intended to receive both vaccines (78). Another study examined the impact of physician recommendations delivered by phone call or in face-to-face interviews among adults ≥65 years. Although 24.5% of participants (n=200) were aware of the pneumococcal vaccine, only 5 (2.5%) had been vaccinated. Among the 97 patients contacted by phone, 58 (59.8%) received pneumococcal vaccination, whereas 84 (81.6%) of the 103 interviewed face-to-face received the vaccine. These findings demonstrate that physician-delivered information significantly increases vaccination uptake (85).
Arya et al. (86) conducted a systematic review of adult pneumococcal vaccination across 31 European countries and found that sequential vaccination (PPSV23 followed by PCV) is recommended for adults in many NIPs. The primary rationale for recommending pneumococcal vaccination is its potential to reduce healthcare and economic burdens. Incorporating higher-valency PCVs into adult NIPs is cost-effective. Additionally, higher coverage rates are observed when countries extend their NIPs to include at-risk populations. The authors suggest that these findings may encourage improved surveillance systems and strengthened efforts to reach target populations effectively.
Recommendations
Low pneumococcal vaccination rates among adults contribute to the continued high prevalence of infections caused by vaccine-covered serotypes, despite the protection offered by available vaccines. Research shows that awareness and education campaigns targeting both the public and healthcare professionals effectively increase participation in vaccination programs among older adults and at-risk populations (47,80). The Adult Vaccination Campaign in Europe (ADVICE) was established to raise awareness of adult vaccination across Europe and to better understand the dynamics of vaccination practices and the barriers to achieving target vaccination rates (87).
Kafadar et al. (88) conducted a meta-analysis of interventions designed to reduce vaccine hesitancy in adults (≥18 years) and increase vaccination uptake rates in the United Kingdom (UK). The authors categorized interventions into four main groups: (i) organizational-level; (ii) recipient-oriented; (iii) provider-oriented; and (iv) multidimensional (a combination of the first three). They reported that providing clear and understandable information, along with using a reminder system with personalized messages or letters, were among the most frequently used and most effective strategies. Organizational interventions aimed to improve access by offering vaccinations in alternative locations or at flexible times. Recipient-oriented interventions sought to increase demand through educational programs and encouragement. Provider-oriented interventions included motivational and educational initiatives to reduce hesitancy among healthcare workers and increase their vaccine uptake.
To promote broader acceptance and use of vaccines, several measures can be implemented. These include providing education and training programs on adult vaccination for healthcare providers, offering public consultation services, securing support from community leaders, raising public awareness of vaccine benefits and risks, and strengthening confidence in vaccination. Additional steps include implementing legal measures to address misinformation and disinformation, ensuring the systematic follow-up and maintenance of structured medical records, maintaining an adequate vaccine supply, integrating adult vaccination schedules into the expanded immunization program, and providing vaccines free of charge (70).
It is crucial to recognize that vaccines affect not only individual health but also community-level public health. Health authorities, healthcare professionals, and individuals all share responsibility for increasing adult vaccination rates—particularly pneumococcal vaccination rates— toward optimal levels.
The Republic of Türkiye Ministry of Health takes a cautious approach to sharing health-related data, prioritizing privacy, national security, and legal compliance. Data such as vaccination rates, epidemiological trends, adult vaccination records, pneumococcal disease and LRTI incidence/mortality, and other disease-specific statistics are frequently restricted to safeguard patient confidentiality and prevent misuse. However, these restrictions can hinder comprehensive public health analyses and limit comparative research by external institutions.
Key Recommendations
- Increase adult vaccination uptake to address the burden of pneumococcal infections. A national adult pneumococcal vaccination policy should be established, along with a clear vaccination coverage target.
- Monitor serotype replacement and antimicrobial resistance to guide vaccination strategies. This requires maintaining an active and effective surveillance system to inform a dynamic pneumococcal vaccination policy.
- Strengthen primary care engagement, while increasing the number of adult vaccination outpatient clinics and units to facilitate easier access. These centers must maintain an adequate supply of vaccines.
- Engage occupational medicine units actively in vaccination efforts.
- Use healthcare encounters —including outpatient visits, hospitalizations, and home healthcare—as opportunities for pneumococcal catch-up vaccination.
- Implement electronic vaccination cards for adults to enable both individuals and healthcare providers to track vaccination status.
- Ensure electronic documentation for vaccines obtained directly from pharmacies and administered outside registered facilities, so that they are properly recorded in national healthcare registries.
- Expand education and training opportunities for the community and healthcare providers (e.g., physicians, nurses, midwives, and pharmacists) delivered through congresses, symposia, conferences, in-service training courses, and online programs.
- Foster collaboration between health authorities, public and private hospitals, and patient organizations to build a strong, effective vaccination ecosystem.
- Adopt continuous social-listening practices to encourage vaccination and address misinformation across all media platforms.
- Vaccinate healthcare professionals with risk factors, helping build trusted role models and increasing public confidence.
- Leverage electronic patient follow-up platforms (such as E-nabız in Türkiye) to send vaccination reminders directly to individuals with vaccine indications, recognizing that physician-directed reminders may be limited by time constraints.
- Send positively framed SMS reminders (e.g., “Protect Yourself”) to high-risk groups and older adults to maintain awareness and encourage vaccination.
Conclusion
Invasive pneumococcal disease remains a major cause of morbidity and mortality in adults, particularly in older adults and those with underlying conditions. Pneumococcal vaccines provide effective protection against the disease and its complications, and rising antimicrobial resistance among S. pneumoniae isolates further underscores their importance. Numerous studies demonstrate the cost-effectiveness of pneumococcal vaccination in adult populations However, adult vaccination rates remain low. Improving awareness among healthcare professionals and the public, strengthening confidence in vaccines, and ensuring equitable access are essential steps toward increasing coverage. Ultimately, timely vaccination should be recognized as a fundamental component of lifelong health and protection.