Introduction
Pityriasis rubra pilaris (PRP) is a papulosquamous disease of unknown etiology that progresses from keratoderma to erythroderma, particularly affecting the palms and soles. It is classified into five subtypes. The form associated with human immunodeficiency virus (HIV) infection is defined as type 6 (1). Pityriasis rubra pilaris type 6 is characterized by the presence of HIV infection, usually accompanied by findings of immunosuppression, a poor prognosis, and a poor response to etretinate; variably, it may be associated with acne conglobata, hidradenitis suppurativa, and lichen spinulosus lesions (2). In this report, we present a case of PRP type 6, which is the first case in Türkiye to be successfully treated with antiretroviral therapy (ART) and retinoid.
Case
A 22-year-old homosexual male presented to the infectious diseases outpatient clinic with rashes and thin, crusted peeling on both knees and elbows. He had no known medical conditions and was not taking any medications. Physical examination revealed multiple orange-brown, scaly plaques on the flexor surface of the elbows (Figure 1). The palms, soles, and oral mucosa were normal. Nails were regular, and there was no lymphadenopathy.
An HIV test was performed considering the patient’s sexual history and was reported positive. A biopsy specimen was taken from lesions with a hyperemic appearance on admission, and ART with tenofovir alafenamide/emtricitabine/bictegravir (TAF/FTC/BIC) was initiated. There were no signs of significant immunosuppression. Routine laboratory tests were within normal limits. The CD4+ T lymphocyte count was 522 /µL, and the viral load was 19,100 copies/mL. No opportunistic infections or malignancies were identified, and prophylactic treatment was not recommended. Serologic testing using the Venereal Disease Research Laboratory (VDRL) test and Treponema Pallidum Hemagglutination Assay (TPHA) was negative.
By the first month of treatment, the hyperemic appearance in the knees and elbows persisted with partial improvement. In the second month, desquamative follicular papules spread from the back to the anterior trunk, chest, neck, and scalp, accompanied by bilateral peeling on the hands and feet (Figure 2).
A punch biopsy specimen taken from the right knee revealed superficial dermatitis with alternating parakeratosis, follicular plug formation, acanthosis, and focal hypogranulosis. Another punch biopsy specimen from the back revealed acanthosis in the epidermis and mild fibrosis in the dermis, compatible with PRP. Dermatologist initiated a retinoid drug acitretin 25 mg/day.
Written informed consent was obtained from the patient for the publication of his medical history, diagnosis, clinical findings, and treatment results.
Discussion
Pityriasis rubra pilaris usually presents as a burning, scaly, and painful erythrodermic rash composed of follicular papules that coalesce into plaques. It frequently affects young men, both homosexual and heterosexual. The pathogenesis of PRP type 6 is believed to be related to an abnormal immune response to antigenic triggers, most notably HIV, and follicular inflammation caused by HIV infection of the hair bulge area. Vitamin A deficiency, retinol-binding protein deficiency, and genetic factors may also contribute to the causation (3).
There is no definitive laboratory test or genetic marker for diagnosing PRP. As in our patient, the diagnosisrelies on clinical suspicion and dermatopathologic correlation since nodulocystic folliculitis differentiates PRP type 6 from classical forms of PRP. Several cases of HIV-associated PRP have been reported in the literature (3-5), with the onset of PRP occurring shortly after or concurrently with HIV diagnosis.
In the present case, the patient was unaware of his HIV status and had no other known immunosuppressive disease. Pityriasis rubra pilaris is among conditions that definitely should be considered in people living with HIV, particularly in men who have sex with men, but also in heterosexual males presenting with follicular and/or papular rashes.
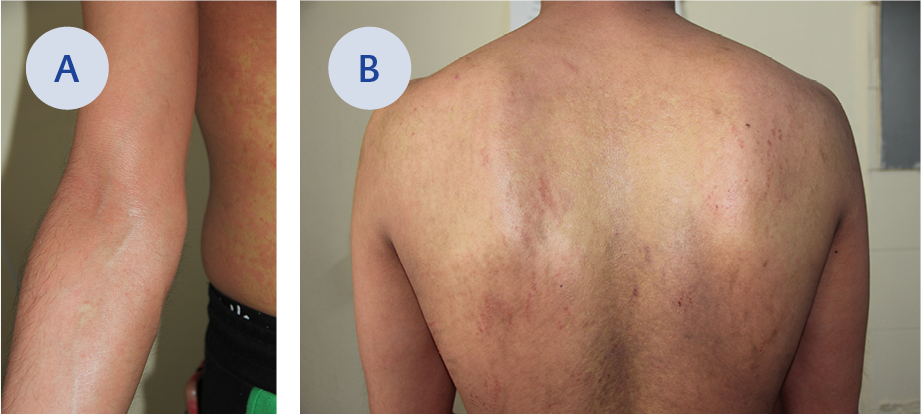
Figure 3A. Clinical appearance after three months of treatment (elbow and flank).
Figure 3B. Clinical appearance after three months of treatment (back).
The primary treatment modality for PRP type 6 is antiretroviral therapy, which can alleviate symptoms and even lead to complete regression in many patients, as seen in our patient after three months (Figures 3A and 3B). This case underscores the importance of effective and concerted ART in managing PRP type 6.
Conclusion
With this case report, we aimed to draw attention to this HIV-associated skin rash because PRP type 6 is rare; it is the first case in Türkiye. It may occur independent of immunosuppression, and in some cases, it responds late to retinoid therapy. Early recognition and management are essential for optimal outcomes.

