Introduction
After the declaration of the pandemic on March 11, 2020, by the World Health Organization (WHO), approximately 771 million people were affected by COVID-19 globally, and about 7 million deaths have occurred as of the third week of November 2023 (1, 2). In Turkey, the first COVID-19 case was identified on March 11, 2020, and as of March 2023, approximately 17 million people were infected, and 102,000 have died (3). Turkey ranks 12th among all countries worldwide regarding cumulative cases (2). Due to the lack of a broad-based study on healthcare workers (HCWs) in our country, based on official statements, 7428 HCWs were reported to be infected with COVID-19 in April 2020 and 29,865 in September 2020. Compared to the general population, the numbers were 4.95 and 8.48 times more frequent in HCWs (4, 5).
The declaration of the COVID-19 pandemic was unprecedented for HCWs worldwide. Since HCWs were at the forefront of the pandemic struggle, they became vulnerable (6). They were not only an important at-risk group in terms of being infected due to the viral load they faced, but they were also exposed to a huge workload (7). During the COVID-19 pandemic in Turkey, the routine clinical practices of HCWs changed significantly; a wide range of services was provided, and many HCWs’ regular jobs, workplaces, or office settings had to change (8, 9). In addition to all the existing health services, contact tracing or filiation studies started. Many new healthcare needs arose, including isolation of patients infected with COVID-19, quarantine of contacts, supply of medicines, mobile vaccination services, COVID-19 outpatient and inpatient clinics, and intensive care units. In addition to all these, factors such as the fear of transmitting the disease to family members, family-work conflict, taking self-isolation measures, efforts to balance their duties to their patients, their responsibilities to their families (e.g., living apart from the family to prevent the transmission of the infection to family members), deaths among colleagues, and long-term use of protective equipment were potential triggers of mental health problems in HCWs, including generalized anxiety disorder and depression (10).
An increase in mental health problems among HCWs during the COVID-19 pandemic was reported in the literature. For example, a study conducted in Turkey revealed that 54.4% of HCWs experienced depression and 51.9% anxiety (11). HCWs may have become vulnerable because they were concerned about their working conditions as well as the health of themselves and their loved ones. From this point of view, our study aimed to determine the depression, anxiety, and stress levels of HCWs actively working during the COVID-19 pandemic at the end of the second year of the pandemic.
Materials and Methods
This cross-sectional study was conducted in Ankara at the Provincial Health Directorate Numune Campus between January and April 2022. Approximately 800 HCWs were working on the Numune Campus during the study period. They were visited during working days and hours, and the study’s questionnaire forms were distributed to those who volunteered to participate and gave consent.
Considering a probable increase in the frequency of mental health problems during the pandemic, the frequency of anxiety was expected at 50%, and the sample size was calculated as 363 using the OpenEpi statistical package program (12), with a confidence interval of 99% and a margin of error of 5%.
The study data were collected by a questionnaire form prepared by the researchers. The questionnaire consisted of two parts: 1) the socio-demographic characteristics, self-history, and working characteristics of each HCW; 2) the Depression, Anxiety, and Stress Scale (DASS-21).
The original DASS was developed by Lovibond in 1995 and consists of 42 questions (13). A 21-question short form of the scale was developed by Antony et al. in 1998 (14). The Turkish validity and reliability of DASS-21 was performed by Yılmaz et al. in 2017; the Cronbach alpha coefficient of the scale was reported as 0.808 for depression, 0.819 for anxiety, and 0.755 for stress (15). DASS-21 is a 4-point Likert-type self-report scale that examines anxiety, depression, and stress dimensions, each subscale consisting of seven items used in clinical and non-clinical samples.
Responses to the scale are scored as “did not apply to me at all” given 0 points; “applied to me to some degree, or some of the time” given 1 point; “applied to me to a considerable degree or a good part of the time” given 2 points; and “applied to me very much or most of the time” given 3 points. The scores of each sub-dimension range from 0 to 21, and as the score obtained from the sub-dimensions increases, the level of depression, anxiety, or stress increases. Completing the questionnaire took 15 to 20 minutes. An Institutional Review Board approval (file number: 2021-12/20) was obtained following official permission from Ankara’s Provincial Health Directorate.
The statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) 20.0 (IBM Corp., Armonk, NY, USA). Descriptive information about the study group was presented with numbers, percentages, standard deviations, and means. The Shapiro-Wilk test was used to test the normality of the data. Mann-Whitney U or Kruskal Wallis tests and Spearman correlation analysis were performed for the univariate data analyses. For multivariate analysis, the logarithm of the score obtained from the DASS-21 scale was taken according to the base “e,” and multiple linear regression analysis was applied. The statistical significance was set as p<0.05.
Results
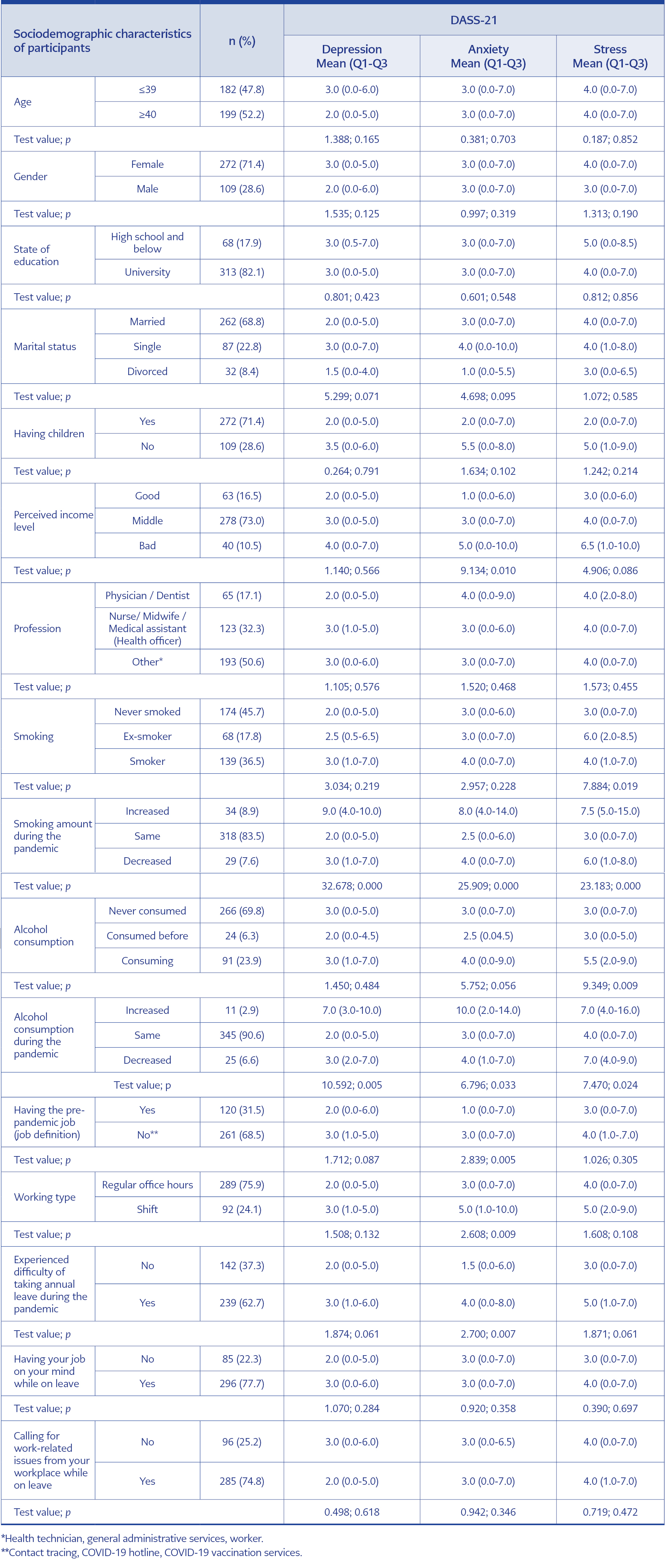
Of the 381 participants included in the study, 272 (71.4%) were female, and 109 (28.6%) were male. Their ages ranged from 21.0 to 63.0, with a mean (SD) of 40.0 (10.0) and a median of 40.0. The anxiety level of the participants with a low perceived income level and the depression, anxiety, and stress levels of those whose smoking and alcohol use increased during the pandemic were comparatively higher (p<0.05 for each). The comparisons of the socio-demographic characteristics of HCWs and the scores they received on the DASS-21 scale are shown in Table 1.
The results revealed that 44.9% (n=171) of the HCWs were infected with COVID-19 at some point. While 51.4% of those with a COVID-19 infection completed the isolation process and received treatment at home, 5.3% were hospitalized, and 43.3% did not receive treatment.
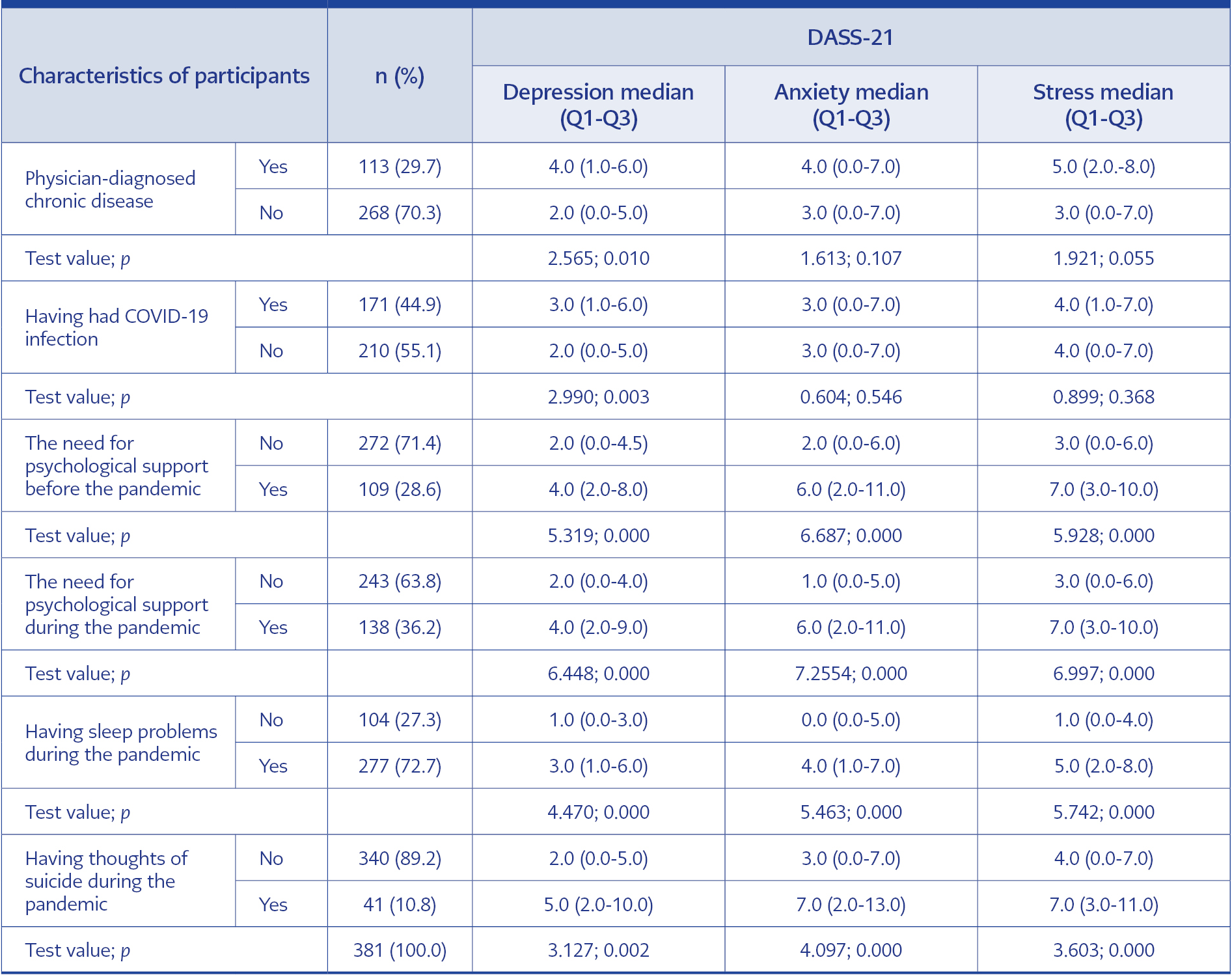
Of the participants, 37.3% stated they felt tired-exhausted, 30.2% anxious, and 12.1% unhappy-devastated. It was detected that the need for psychological support increased during the pandemic period compared to the pre-pandemic period (28.6% vs. 36.2%) (p<0.001). Those who needed psychological support before and during the pandemic, those who had sleep problems, and those who had suicidal thoughts got higher scores on the DASS-21 (p<0.05 for each group). Although those with sleep problems had higher scores on the DASS-21, the prevalence of sleep problems was also higher in health workers with symptoms of depression, anxiety, or stress (p<0.05 for each). The comparisons of participants’ characteristics and DASS-21 scores are presented in Table 2.
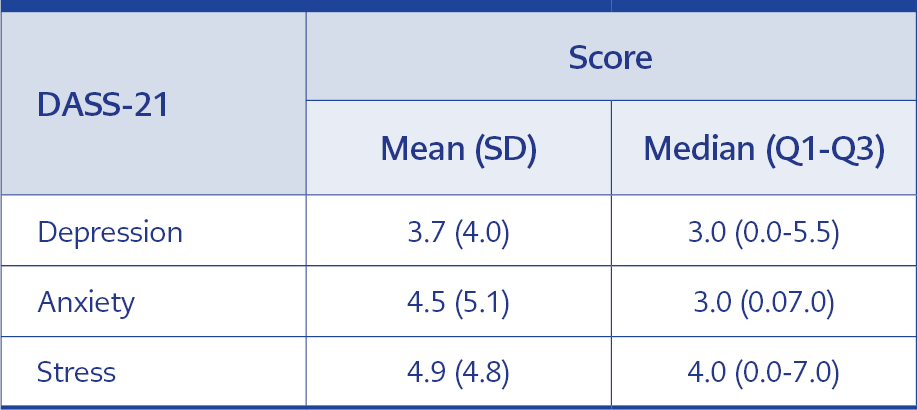
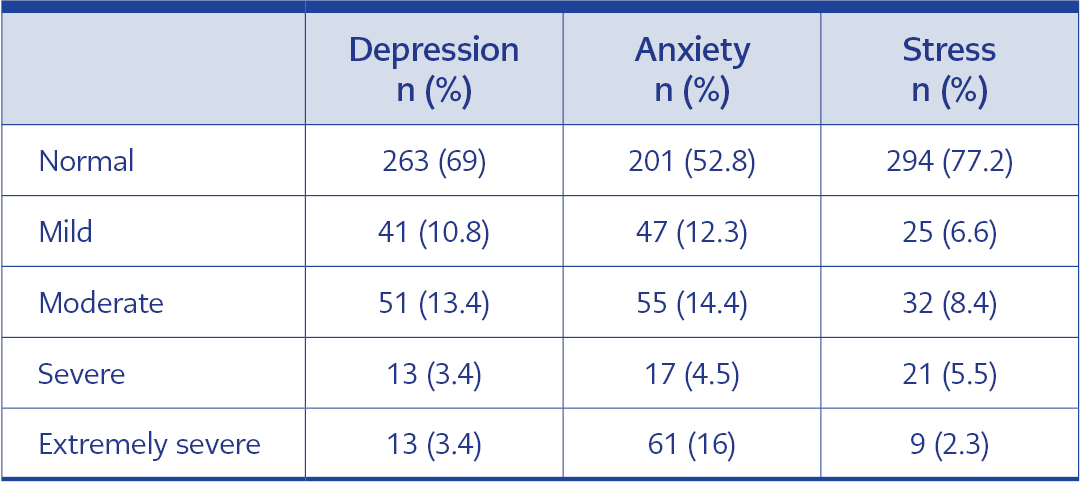
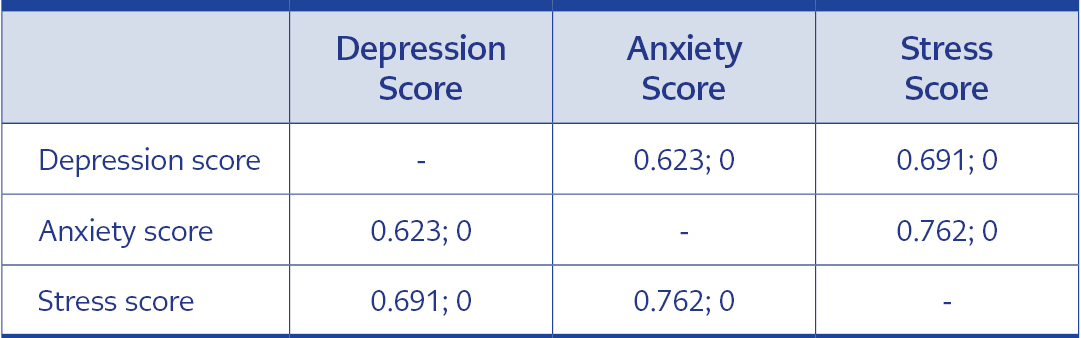
According to one of the DASS-21 subscales, 31% of the participants showed depressive symptoms ranging from mild to extremely severe. There was a positive correlation between all three domains of the DASS-21 (p<0.001 for each). DASS-21 scores of participants are shown in Table 3, and the frequency of depression, anxiety, and stress severity is in Table 4. The correlation values of sub-dimensions are presented in Table 5.
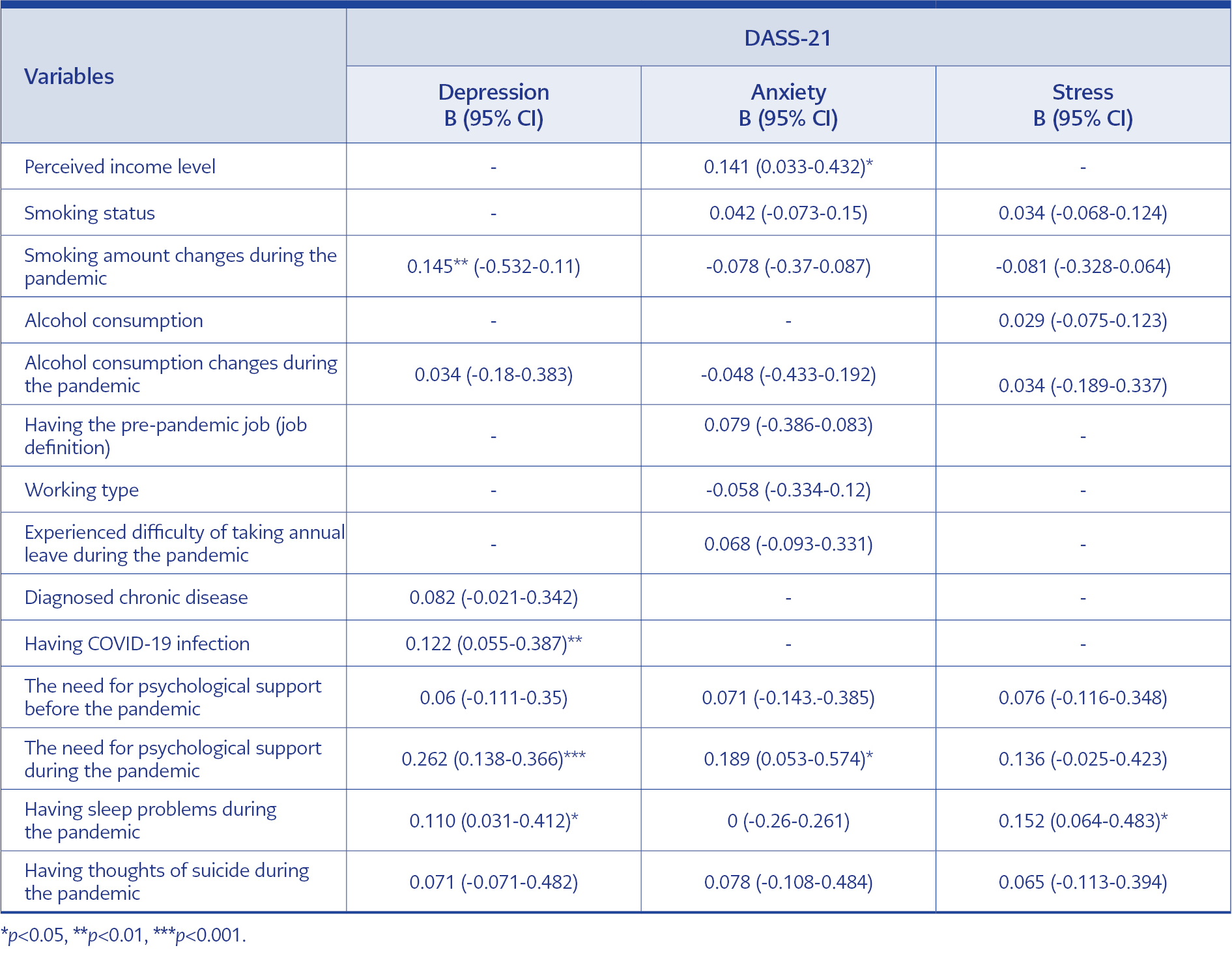
According to our multivariate analysis, anxiety scores were relatively higher in those with both low perceived income and who professed the need for psychological support during the pandemic (p<0.05 for each). Depression scores were higher in those whose smoking amount increased during the pandemic, those who had a COVID-19 infection, those who had sleep problems, and those who needed psychological support (p<0.05 for each). Multivariate analysis results are given in Table 6.
Discussion
Although COVID-19 no longer constitutes a public health emergency of international concern (16), many people are still infected with the virus. Sometimes, the clinical course may result in severe illness and death. In addition to the increasing workload, many factors, such as the risk of being exposed to a highly contagious and deadly virus every day, the thought of transmitting the virus to family members, and the stress and fatigue caused by having to respond quickly to increasing needs continue to affect the mental health of HCWs negatively (10). From this point of view, the present study aimed to determine the depression, anxiety, and stress levels of HCWs during the pandemic.
COVID-19 has adverse effects on the mental health of millions of people, as well as their physical health. Factors such as social isolation, being infected with the virus and the thought of infecting family members, and economic changes triggered by the pandemic have caused a global increase in the frequency of negative psychological reactions such as depression, anxiety, post-traumatic stress disorder, and suicide (17, 18). The COVID-19 pandemic, one of the most important public health crises of the last century, in addition to its effects on society, has put HCWs, who have been working on the front lines and under excessive workload since the first moments, in the highest risk group in terms of mental health problems.
The emotional reactions of HCWs during the COVID-19 pandemic are complicated. The reasons that led to an increase in the frequency of mental problems among HCWs can be listed as follows: the increase in professional responsibilities, prolonged working hours, long and close contact with positive cases, the thought of catching the virus themselves and their family members, encountering a new factor, uncertain medical treatments, lack of vaccination (especially in the first pandemic periods), and the persistency of a high case-rate for a long time till reaching herd immunity. Previous studies have shown that mental health problems such as anxiety and depression are frequent among HCWs (19). For example, in a study by Uz et al. conducted during the early period of the COVID-19 pandemic in Turkey, the frequency of depression was found to be 39.8%, and the frequency of anxiety was 26.2% (20). An online study by Şahin et al. reported that 77.6% of HCWs exhibited symptoms of depression, 60.2% anxiety, and 76.4% distress (21). In another study conducted among primary HCWs before the pandemic in Turkey, depression was reported at 20.7%, anxiety at 27.2%, and stress at 18.2% (22). In addition, in a study conducted on people who were and were not HCWs during the pandemic in Turkey, Hacimusalar et al. reported that mental problems such as anxiety and hopelessness were higher among HCWs (23). A cross-sectional study from China by Lai et al., including 1257 HCWs in 34 hospitals, revealed that 50.4% of the HCWs had depression, 44.6% anxiety, and 71.5% stress symptoms (17). Another study from Italy by Rossi et al. reported the frequency of depression at 24.7%, anxiety at 8.3%, and stress at 21.9% (24).
Our study was conducted in the second period of the pandemic, and we found the frequency of depression to be 31.0%, the frequency of anxiety 47.2%, and the frequency of stress 22.8%. We think the different frequency rates between the studies may stem from the pandemic periods in which the studies were conducted, the effects of the changing and prolonged period on human psychology, and the fact that the research groups were working at different levels of the health system, such as hospitals and primary care.
We found no relationship between socio-demographic characteristics such as age, gender, marital status, education level, and depression, anxiety, or stress scores. The study by Şahin et al. found that female gender was a risk factor for depression, anxiety, and stress, and age was a risk factor for depression (21). The study by Liu et al., similar to our findings, showed that factors such as age, gender, marital status, and education level were not associated with anxiety in HCWs (26). In contrast, in the study of Lai et al., being a woman was a risk factor for depression, anxiety, and stress (17). In the study conducted by Uz et al., depression, anxiety, and burnout scores were lower in those with higher education levels (20). A systematic review and meta-analysis by Aymerich et al. found no relationship between demographic data such as gender, age, and the frequency of anxiety, depression, and stress (6). Contrary to our findings, the female gender is generally accepted as a risk factor for mental health problems, and higher education levels are associated with mental well-being in the literature. Especially during the periods when the number of cases in the pandemic was high, many doctors, nurses, and all other HCWs worked collaboratively and intensively with a team concept. Facing all the challenges together may have eliminated the effects of gender and age on healthcare teams.
HCWs, who had a critical role in managing the pandemic, took an active role in direct patient care and filiation studies, taking public health measures to prevent the infodemic and guide society correctly. In addition to the social and economic effects of the pandemic on the whole society, the increasing professional burden and increasingly difficult working conditions may have affected the lifestyle behaviors of HCWs and increased the use of substances such as smoking and alcohol. Studies on both the community and health professionals have shown that psychological stressors, public health, and economic crises increase the rates of alcohol and other substance use (26-29). In the systematic review by Rehm et al. on the possible effects of the COVID-19 pandemic on alcohol use, it was shown that psychological factors might worsen patterns of addictive substance use (27). Similarly, our findings showed that the depression, anxiety, and stress scores of people who increased smoking and alcohol consumption during the pandemic were higher. A systematic review by Roberts et al. showed that the use of alcohol and other substances increased during the pandemic; it was reported that the increase in the use of alcohol and other substances was related to anxiety, unhappiness, and social isolation, and the most common mental health problem associated with this increase was depression (28). A study conducted on HCWs in Ethiopia showed a relationship between alcohol and cigarette use and psychological stress, which supports our findings.
On the other hand, in another study conducted among HCWs in Kenya, alcohol use was not associated with psychological problems such as depression and anxiety (29, 30). In our study, alcohol use was questioned based on the participants’ declaration without specifying the time. The study conducted in Kenya evaluated it in terms of alcohol use disorder and analyzed it accordingly, which may have contributed to different results. Our cross-sectional study cannot answer the question of whether mental problems affect smoking and alcohol use or whether these problems are more common in smokers. Although we could not demonstrate the cause-effect relationship, our study presented a relationship between increased smoking and alcohol use and mental health problems.
The univariate analyses in our study showed that patients with chronic diseases reported higher scores on the depression subscale; however, this relationship could not be shown for anxiety and stress. In the study of Uz et al., no relationship was reported with comorbid diseases (20). When we looked at the other background characteristics, depression, anxiety, and stress levels were seen as higher in those who needed psychological support before and during the pandemic and those who had sleep problems and suicidal thoughts. The relationship between sleep and psychiatric issues is complex. In the literature, it has been reported that in most patients with psychiatric problems, there is a significant decrease in sleep efficiency and total sleep time. On the other hand, mental problems such as depression, anxiety, stress, and decreased self-esteem occur with decreased sleep quality (31, 32). Although the causal relationship between sleep and psychiatric problems could not be demonstrated in our study, the existence of a relationship, even in multivariate analyses, suggests that it will pave the way for studies with different designs.
In our study, although depression scores were higher in those with a history of chronic disease in univariate analyses, this could not be shown in multivariate analyses. A similar result was reported in another study conducted in Turkey by Şahin et al. (21). In the study of Li et al., it was shown that mental health problems are more common in women HCWs with a chronic disease and a history of psychiatric disorder (33). A study conducted in China during the first period of the pandemic showed that having an organic disease is a risk factor for psychological problems such as anxiety, depression, and insomnia in HCWs (34). A multi-centered study by Asnakew et al. showed a relationship between medical illness and depression but not with anxiety (35). In our study, the fact that only 30% of HCWs had chronic diseases, especially the practices such as keeping individuals with chronic diseases, which may have a high mortality rate in COVID-19 infection, in the background of COVID-19-related studies and considering them on administrative leave may have been effective in the formation of these results.
Our study has some limitations. The most important limitation is the cross-sectional design of the study. In addition, we did not use any sampling method; the participants being volunteers may cause selection bias. The self-reported and recall-based responses may cause recall bias. These biases may have affected our results.
In conclusion, our study showed that the frequency of depression, anxiety, and stress was found to be high in HCWs who took an active role in the COVID-19 pandemic in Turkey. The need for psychological support and the frequency of smoking and alcohol use, which were shown to be associated with depression, anxiety, and stress, increased compared to the pre-pandemic period. One out of three HCWs reported experiencing mental health problems. It is essential to improve the working conditions of HCWs to help them cope with the effects of the pandemic on their mental health and to provide psychosocial support.