Introduction
Inherited defects in the adenosine deaminase (ADA) gene result in severe combined immunodeficiency (ADA-SCID). Cytopenias caused by autoimmune disorders or bone marrow failure occur in 50% of patients, presenting as pure red cell aplasia, neutropenia, thrombocytopenia, or pancytopenia. Other complications include hypogammaglobulinemia, recurrent infections, and immune deficiency associated with malignant lymphoproliferation (e.g., T-large granular lymphocyte leukemia and lymphoma). Hematopoietic stem cell transplantation (HSCT) is the standard treatment for ADA-SCID; however, patients who are unable to undergo transplantation remain highly susceptible to opportunistic infections (1).
Aspergillus species, particularly Aspergillus flavus, are among the most common causes of invasive aspergillosis (IA) in immunocompromised patients, contributing to high morbidity and mortality. Voriconazole is the first-line treatment for IA, even in cases with extrapulmonary involvement (2). Breakthrough infections caused by non-fumigatus Aspergillus, non-albicans Candida, Mucorales, and other rare pathogens are associated with significantly high mortality rates, underscoring the need for aggressive diagnostic and therapeutic approaches (3).
This case report describes a patient with ADA-2 deficiency who developed IA due to A. flavus. Despite multiple therapeutic interventions, including antifungal therapy and surgical procedures, the infection progressed and proved fatal.
Case
A 13-year-old male with ADA-2 deficiency due to a homozygous CECR1 (c.11104 del) mutation was referred to our center for HSCT because of the ongoing war in his home country. At the age of 10, he had been diagnosed with nodular sclerosis Hodgkin lymphoma and had undergone chemotherapy. During treatment, he developed ileus requiring ileostomy. Further history revealed parental consanguinity, and his twin sibling had previously undergone HSCT for aplastic anemia but had unfortunately passed away post-transplantation.
The patient was on a regimen of adalimumab (20 mg weekly), methotrexate (15 mg weekly), and monthly intravenous immunoglobulin (0.5 g/kg). On presentation, clinical examination revealed growth retardation, hepatosplenomegaly, and an ileostomy. Other aspects of his physical examination were unremarkable. Laboratory investigations revealed: white blood cell (WBC) count 2020/mm³, neutrophils 1080/mm³, lymphocytes 490/mm³, hemoglobin (Hb) 3.9 g/dL, platelets 67,000/mm³, aspartate aminotransferase (AST) 129 IU/L, alanine aminotransferase (ALT) 142 IU/L, and ferritin 1104 µg/L. Bone marrow aspiration demonstrated pure red cell aplasia and overall bone marrow hypoplasia, necessitating HSCT. However, no compatible family donor was available, prompting a search for unrelated donors.
The patient had received the Bacillus Calmette-Guérin (BCG) vaccine in his home country, and the interferon-gamma release assay (IGRA) was negative. Anti-tuberculosis prophylaxis was initiated with isoniazid (10 mg/kg/day) and rifampicin (15 mg/kg/day). Due to recurrent abnormalities in liver function tests, the regimen was modified to ethambutol (20 mg/kg/day) and levofloxacin (750 mg/day). Unfortunately, the identified non-domestic donor later withdrew from donation.
The patient subsequently developed a one-week history of fever, herpetic lesions below the left eye, and persistent pruritic maculopapular lesions on the legs and face, accompanied by mild erythema and swelling of the left cheek and periorbital area. Bacterial-viral respiratory polymerase chain reaction (PCR) panel, serum sepsis PCR panel, galactomannan test, and cultures from peripheral catheter blood and urine were all negative. Abdominal ultrasonography (USG) revealed hepatosplenomegaly without additional abnormalities. Chest computed tomography (CT) showed normal lung parenchyma. Skin biopsy did not reveal findings suggestive of a specific pathogen. Liposomal amphotericin-B (L-AmB, 3 mg/kg/day) was added to the broad-spectrum antibiotics the patient was already receiving.
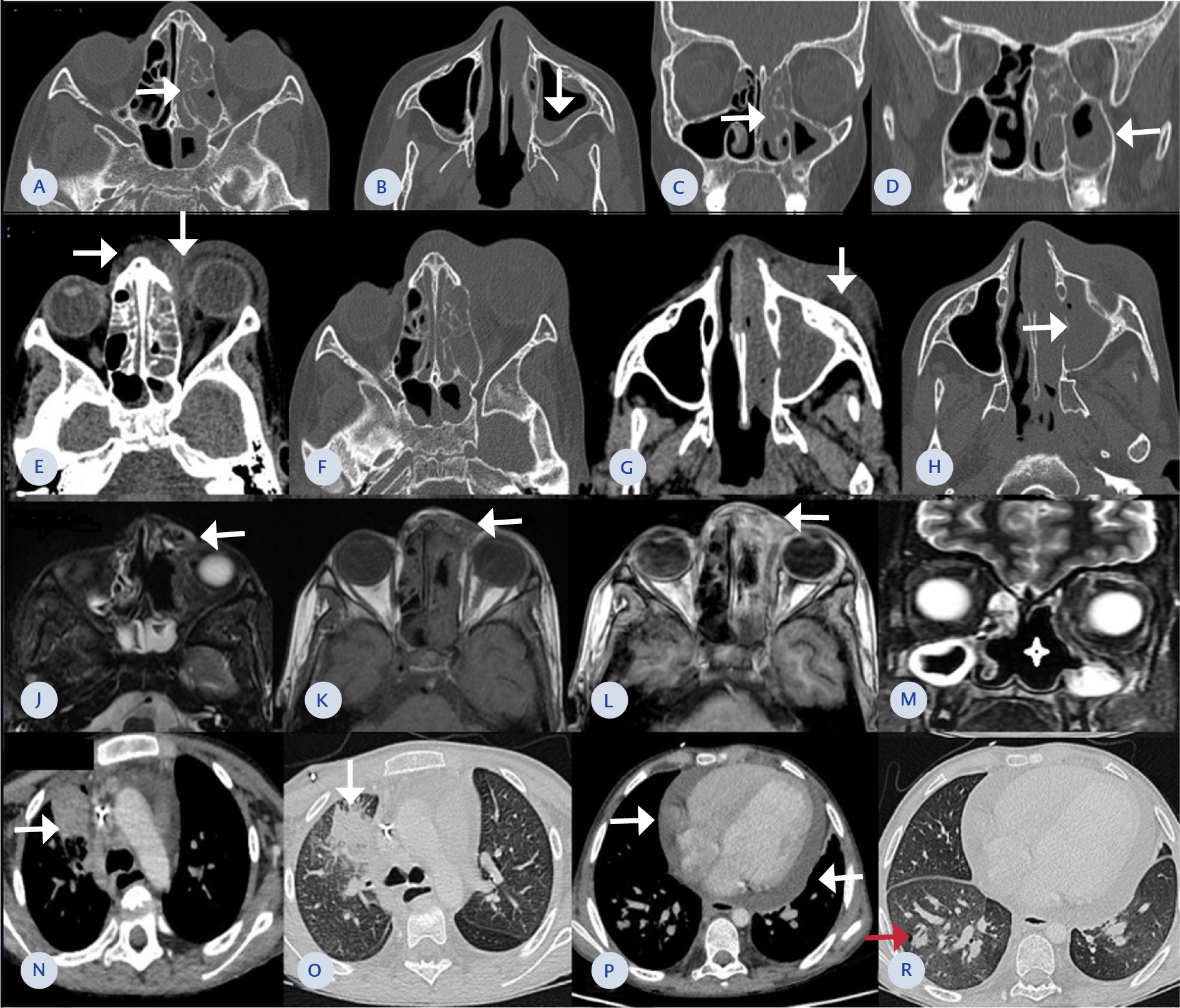
Figure 1. (A-D) Paranasal sinus CT images show loss of ventilation and soft tissue density material in the left ethmoid cells and sphenoid sinus. An air-fluid level is observed in the left maxillary sinus (arrows), accompanied by mucosal thickening. These findings are consistent with chronic sinusitis. No signs of fungal infection, such as high-density material or bone destruction, were present.
(E-H) Orbital CT images reveal soft tissue thickening in the left eyelid and periorbital area. The inflammation extends into the orbital cavity through the postseptal space in the medial orbit (arrows; E), resulting in a proptotic appearance of the left eye. Inflammation also extends toward the nasal root (arrows; A). A limited subcutaneous collection, suggesting an abscess, is noted in the right maxillary area (arrow; G). The right maxillary sinus is filled with soft tissue density, and thinning of its medial wall is observed (arrows; H).
(J-M) Facial MRI shows regression of inflammation in the left ethmoid sinuses. However, subcutaneous inflammation persists on the nasal side of the left periorbital region (arrows; J, K, L). Inflammation in the left orbit has decreased. Destruction is noted in the nasal septum and middle turbinates (asterisk; M). Mucosal thickening persists in the maxillary sinuses.
(N-R) Thorax CT images show improved homogeneity of parenchymal aeration. An irregular consolidation adjacent to the mediastinum is seen in the anterior segment of the right upper lobe, with surrounding ground-glass opacity (arrows; N, O). Pericardial effusion is present (arrows; P). A peripheral, peribronchial nodular lesion is observed in the posterobasal region of the right lower lobe (red arrow; R).
During follow-up, swelling and erythema around the left eye worsened, accompanied by persistent fever. Paranasal CT demonstrated reduced air content and significant thinning of the bone structures, with peripheral mucosal thickening observed in both maxillary sinuses, anterior and posterior ethmoidal cells, and other sinus compartments (Figure 1. A-D). Orbital CT was consistent with preseptal cellulitis. Nasal endoscopy revealed minimal dryness, and a biopsy was taken from the affected area. Preliminary pathology showed necrotic fungal structures, including both septate and non-septate forms, primarily suggesting mucormycosis. However, the sample could not be definitively interpreted due to ongoing antifungal treatment.
Functional endoscopic sinus surgery (FESS) was subsequently performed. During the surgery, crusted lesions were observed on the anterior surface of the right middle turbinate, with mucosal color changes noted at the junction of the right septum and middle turbinate (1.5 cm) and on the left nasal passage (2×1.5 cm). The left periorbital region exhibited diffuse swelling, with absent eye movement and a “frozen” eye, findings consistent with mucormycosis. Treatment was intensified with L-AmB (5 mg/kg/day), posaconazole (2×300 mg loading dose followed by 1×300 mg maintenance dose), and intranasal L-AmB (50 mg L-AmB added to 500 mL of saline, 20 cc administered into each nasal cavity every 2 hours).
Despite these interventions, the absolute neutrophil count (ANC) remained <100 cells/mm³, and repeated granulocyte transfusions failed to increase it. Ocular symptoms continued to worsen. Orbital CT revealed progression from left preseptal cellulitis to orbital cellulitis, with worsening sinusitis findings. Inflammation had extended into the orbital cavity, involving the postseptal region (Figure 1.E-H). Exenteration surgery was discussed with the family, but they declined the procedure despite vision loss. A revision FESS was performed, including cavity debridement, left orbital decompression, abscess drainage, and left medial maxillectomy. The L-AmB dose was increased to 10 mg/kg/day.
On day 10 of dual antifungal therapy, orbital magnetic resonance imaging (MRI) demonstrated decreased left exophthalmos and regression of pansinusitis. Fungal culture from the biopsy was positive for Aspergillus spp., and PCR confirmed A. flavus. The histopathological classification revealed angioinvasion. The antifungal regimen was adjusted to L-AmB (10 mg/kg/day), voriconazole (8 mg/kg), and caspofungin (70 mg/day). Weekly voriconazole levels were maintained within the therapeutic range. The frequency of intranasal L-AmB was reduced to eight times daily.
Although the patient initially remained clinically stable, facial swelling and fever recurred on day 49 of antifungal therapy. Magnetic resonance imaging of the face revealed a hypodense, spherical, lobulated abscess (17×12×10 mm) in the left orbital medial area near the nasal root, consistent with abscess formation. The abscess was drained, and fungal cultures returned negative. At the three-month follow-up, inflammation in the left ethmoid sinuses and left orbital space had regressed (Figure 1. J-M). With radiological and clinical improvement, caspofungin was discontinued on day 75.
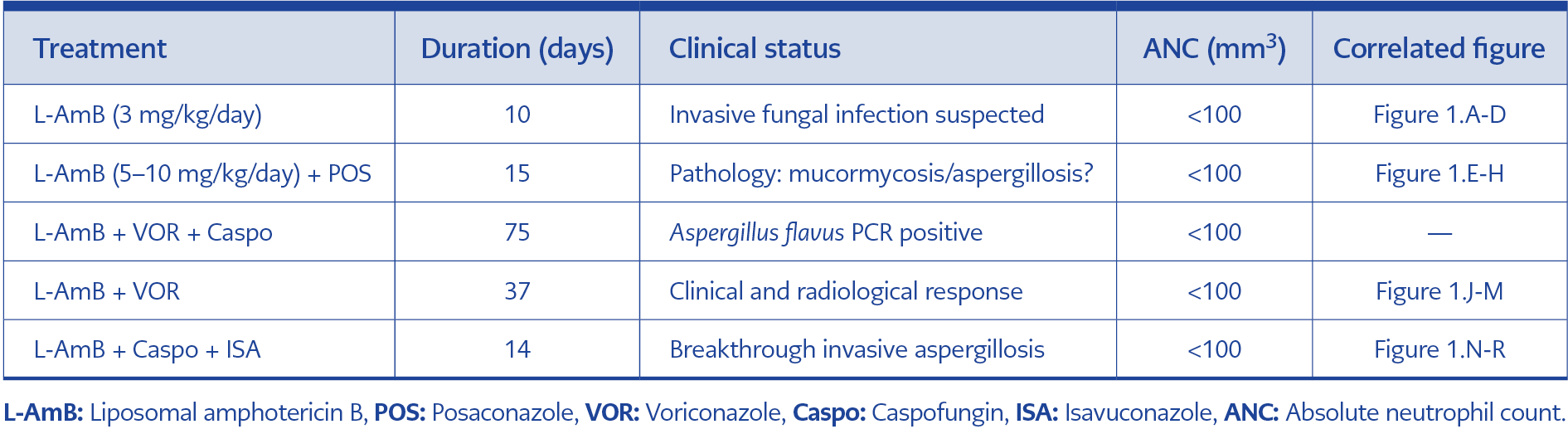
However, on day 137, the patient developed tachypnea and oxygen desaturation. Chest CT revealed a nodular lesion (8×10 mm) adjacent to a vascular structure in the right lower lung lobe, consistent with Aspergillus infection (Figure 1. N-R). Breakthrough IA was diagnosed, and the treatment regimen was adjusted to L-AmB (10 mg/kg/day), caspofungin (70 mg/day), and isavuconazole (200 mg/day, oral). Despite these measures, the patient, who had a severe neutropenia and hypogammaglobulinemia, passed away on day 151 of antifungal treatment. The antifungal combination therapy used in this patient is summarized in Table 1.
Discussion
Primary and breakthrough IA are high-mortality infections, especially in immunocompromised patients, including those undergoing chemotherapy, bone marrow or solid organ transplants, and individuals with primary or secondary immunodeficiencies (4). Culture and histology remain the gold standard for IA diagnosis, while voriconazole is considered the first-line treatment. In cases of breakthrough IA, switching antifungal classes, often to L-AmB, is recommended (2). Combination therapy with azoles such as voriconazole or posaconazole, together with echinocandins, is advised when Aspergillus is identified (5).
In our patient, combination antifungal therapy was initiated due to extensive sinus, bone, and orbital involvement. This approach led to partial clinical and radiological responses. Despite initial improvement, disease progression later necessitated adjustments in the treatment plan.
Antifungal prophylaxis is recommended for patients with bone marrow failure, prolonged neutropenia, and those undergoing HSCT (6). Although echinocandins like caspofungin are generally preferred as first-line empiric therapy in febrile neutropenic patients without mold-active prophylaxis, L-AmB was chosen in this case due to the high clinical suspicion of mold infection, potential mucormycosis involvement, and the presence of cutaneous and orbital lesions, which raised concerns for angioinvasive fungal disease.
Surgical intervention, in addition to antifungal therapy, is often necessary for invasive fungal infections (7). In mucormycosis cases, systemic and local administration of L-AmB has shown some efficacy (8,9). Despite the use of intranasal L-AmB in our patient, fungal vascular invasion hindered antifungal penetration, necessitating further surgical procedures, including extensive sinus debridement and drainage of the orbital abscess.
Initial pathology, culture, and PCR results from FESS specimens demonstrated angioinvasion and growth of A. flavus. The patient was stabilized with combined antifungal therapy, debridement, and local L-AMB irrigation, allowing de-escalation. However, on day 137, the patient’s condition deteriorated with new findings of invasive pulmonary aspergillosis (IPA). By definition, breakthrough IPA refers to any IA that develops during ongoing antifungal exposure, particularly in the context of mold-active prophylaxis, and typically requires a change in antifungal class (10). Accordingly, salvage therapy was promptly initiated; however, the patient unfortunately passed away shortly thereafter.
A 2023 multicenter study in Spain identified non-fumigatus Aspergillus (45.5%) as the most common pathogen in breakthrough fungal infections. Azole resistance was a significant contributing factor, and breakthrough infections were associated with a high mortality rate of 61.4% (3). In our patient, severe neutropenia and hypogammaglobulinemia, along with breakthrough IA due to A. flavus, were key contributors to the fatal outcome.
Antifungal susceptibility testing could not be performed in this case; however, such testing could have provided valuable guidance for clinical management. The resistance profile of the A. flavus subtype to L-AMB or other antifungal agents remains unknown. Anti-tuberculosis prophylaxis is typically managed through a multidisciplinary approach in tertiary centers. While some centers employ isoniazid monotherapy, others prefer a dual regimen combining isoniazid and rifampicin (11). Although our patient received dual prophylaxis, a study involving 12 ADA-SCID cases suggested that isoniazid monotherapy may be an effective alternative (12).
Conclusion
Managing invasive fungal infections in ADA-SCID patients remains challenging due to profound immune dysfunction. This case highlights the challenges of achieving infection control in these patients despite optimal antifungal and surgical interventions. The combination of vascular invasion and underlying immunodeficiency likely contributed to therapeutic failure. Further research is needed to develop more effective treatment strategies for primary immunodeficiencies such as ADA-SCID.