Introduction
The global impact of the coronavirus disease (COVID-19) pandemic has been profound, affecting billions of lives worldwide. As of June 13, 2024, the virus has infected approximately 704 million people and led to a staggering death toll of 7 million (1). In the fight against this devastating virus, the development and distribution of COVID-19 vaccines have been identified as the most crucial strategy to control the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (2). These vaccines have demonstrated varying degrees of effectiveness, with reported rates ranging from 90% to 55% (3-5). Specifically, they have shown to be around 70% effective (95% CI=56-80) in preventing infections, 92% effective (88-94) in reducing hospitalizations, and 91% effective (85-94) in lowering mortality rates (5). Despite these promising results, vaccine acceptance has not been uniform, partly due to concerns about potential unknown effects. Healthcare workers (HCWs), who play a pivotal role in managing pandemic diseases, are considered trusted sources of information for the public, especially regarding aspects such as COVID-19 vaccines (6-8). Their influence extends to their communities and social media platforms, where they can actively combat misinformation and advocate for public vaccination.
The reported rate of COVID-19 vaccine hesitancy among HCWs shows significant variation. The previous study identified this rate in our healthcare settings as 4.5% (9). Despite this low hesitancy rate, this range can increase up to 73%, as documented in several studies (10-12). This variability is influenced by various factors, including age, profession, department, education level, health literacy, knowledge about vaccines, risk perception, and past vaccination attitudes (13-15). For instance, Paterson et al. found different levels of vaccine hesitancy among HCWs in different countries: 6% in Türkiye, 16% in the United States of America (USA), and 2% in Australia (8). However, despite this information, the specific reasons for COVID-19 vaccine hesitancy among HCWs in Türkiye remain unclear. Further research is needed to gain insights into the factors contributing to this hesitancy in the Turkish healthcare context.
Indeed, numerous studies have investigated the determinants of vaccine hesitancy through surveys (16). However, researchers emphasize the importance of conducting qualitative research to gain a deeper understanding of the factors influencing COVID-19 vaccine hesitancy (14, 15, 17). By employing a health promotion model, researchers can potentially achieve more effective and comprehensive results. One such prominent theoretical model used to comprehend and forecast health behaviours is the Health Belief Model (HBM) (18). By applying the HBM in vaccine hesitancy studies, researchers can gain valuable insights into the reasons behind vaccine hesitancy among different populations. Overall, the HBM has proven to be a valuable tool in understanding vaccine hesitancy during the COVID-19 pandemic and can guide public health efforts to improve vaccination rates and combat the spread of the virus (19-21).
In this study, we planned to use qualitative research methods and the HBM approach collectively. HCWs refuse the COVID-19 vaccines despite numerous peer-reviewed studies highlighting the individual and societal benefits of COVID-19 vaccination (5, 22). The study had two main aims: First, to identify the deeper determinants of vaccine hesitancy among HCWs during pandemics, and second, to contribute to the vaccination campaigns in future pandemics with the help of these detailed results.
Materials and Methods
This study was conducted using the qualitative research approach in two pandemic hospitals with a capacity of 650 beds in Istanbul, TÜrkiye. We employed a purposive sampling method for participant recruitment. The term “vaccine-hesitant HCWs” was used to describe individuals over 18 years of age who had not received any COVID-19 vaccines until October 1, 2021 (10 months after the start of Türkiye’s COVID-19 vaccination campaign) and who had not been diagnosed with COVID-19 in the preceding six months. The Occupational Health and Safety Department (OHSD) of these hospitals identified HCWs who had not been vaccinated against COVID-19 (n=23) based on employee vaccination records. All HCWs defined as COVID-19 vaccine hesitant were invited to participate in in-depth, face-to-face interviews via e-mail and phone. Data collection ceased when the interviewers agreed that satisfaction had been achieved (n=13). The interviews, conducted by researchers, lasted 45 ~ 50 minutes, were recorded in an audio recorder and were transcripted by the author within one week. To formulate interview questions about vaccine hesitancy among HCWs, we prepared a semi-structured interview form that adopted the HBM as a conceptual framework. The HBM is frequently utilized by psychologists and health professionals to explore and address harmful behaviours. Its primary objective was to motivate individuals to assess the benefits of modifying harmful behaviours, such as smoking, avoiding immunizations or avoiding exercise to minimize potential health threats. It consists of six distinct components (23), all of which served as a guide in developing the semi-structured interview (see Supplementary and Table 1) conducted during our in-depth interviews with vaccine-hesitant HCWs.
Participants’ written consent was obtained before conducting the interviews, and all sessions were recorded and transcribed verbatim. For the qualitative data analysis, we used MAXQDA 2022 software (VERBI Software, Germany). A codebook created by the researchers was employed to code the transcribed text systematically according to the relevant dimensions. Thematic analysis was conducted to identify common themes emerging from the coded data. The Koç University’s Clinical Research Ethics Committee approved the study on October 13, 2021, with the decision number 2021.375.IRB1.108. Additionally, verbal content was documented in the interview records to ensure comprehensive and accurate data documentation.
Results
Characteristics of Study Participants
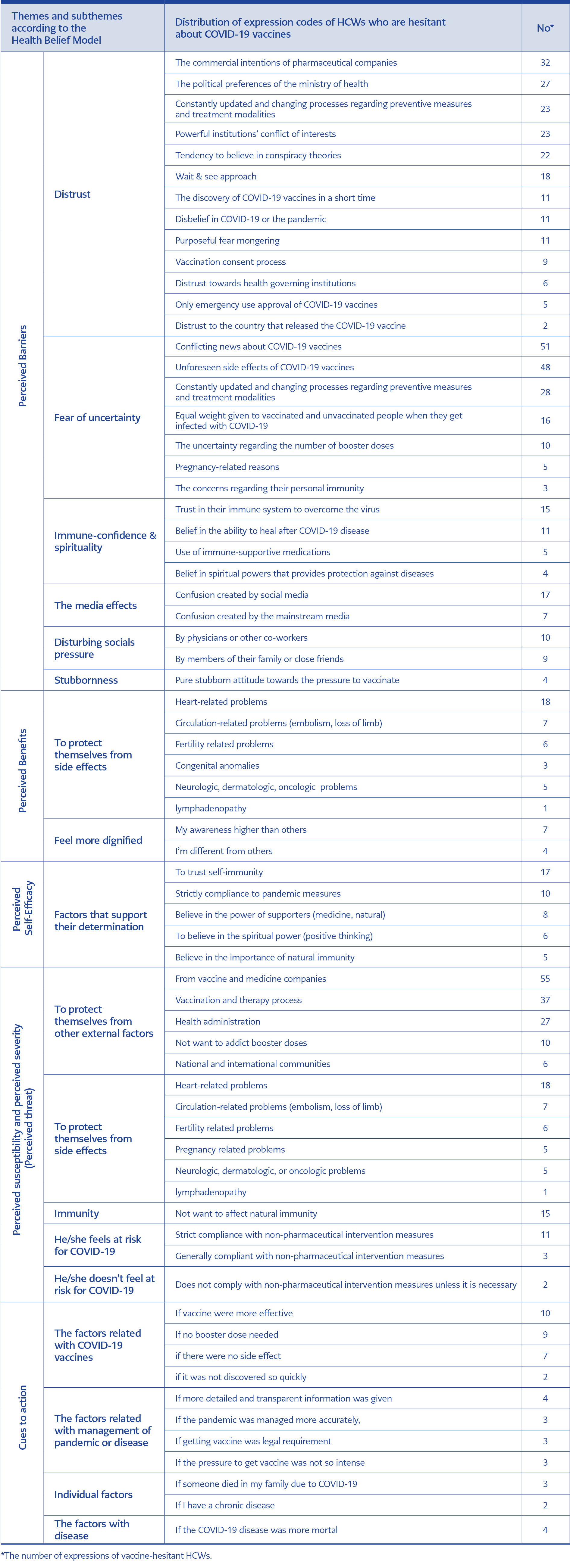
Table 1. Expressions of healthcare workers who are hesitant about COVID-19 vaccines according to the themes and sub-themes of the Health Belief Model.
The study included 13 participants, with a median age of 35 years (ranging from 26 to 48). Eight of the 13 participants were females. Nine of the participants had completed university or higher education, which included master’s or doctorate degrees. Additionally, eight of the participants had no children. Moreover, eight of the participants remained unvaccinated until the interviews were completed.
Perceived Barriers
During the interviews, participants displayed diverse attitudes towards vaccine acceptance. Some HCWs were firmly against COVID-19 vaccines (n=7, 53.84 %), while others expressed hesitation (n=6, 46.15%). Through the data coding process, we identified 29 distinct reasons for COVID-19 vaccine hesitancy (Table 1). These reasons were categorized into six groups: distrust, fear of uncertainty, immune confidence and spirituality, media influence, unsettling social pressure, and obstinacy.
Among these categories, distrust and fear of uncertainty emerged as the primary reasons for COVID-19 vaccine hesitancy among the HCWs. Specifically, the most common codes for vaccine hesitancy were related to “Conflicting news about the effectiveness of COVID-19 vaccines” (51 statements), “Unforeseen side effects of COVID-19 vaccines” (48 statements), and “The commercial intentions of pharmaceutical companies” (32 statements) (Table 1). For instance, one vaccine-hesitant HCW (Participant [P] 8) stated, “I have been following some professors in the media, and some of them advocate for the COVID-19 vaccine, while others are absolutely against it. I see that both groups of physicians have the same medical diplomas and are professionals. I respect them, but their opposite views have left me uncertain and hesitant about getting the vaccine.” Another HCW (P12) expressed concerns about the fluctuating information related to COVID-19 booster doses, saying, “I have heard the news about the COVID-19 booster doses. Initially, scientists advised that the gap between two doses should be 48 days. Then, this period was changed to 36 days, 12 days, and 22 days. How can I trust this constantly changing information? They have not even reached a consensus on a fundamental topic” (Conflicting news about COVID-19 vaccines). Another participant (P11) raised concerns about rumours regarding vaccine side effects, stating, “Some people claim that COVID-19 vaccines can cause infertility and heart attacks. I have read that these vaccines may also lead to skin and circulatory system issues. These types of side effects have become more common after COVID-19 vaccinations” (Unforeseen side effects of COVID-19 vaccines).
Some participants expressed scepticism about the perceived commercial intentions of pharmaceutical or vaccine companies (P12). One participant highlighted their research on the development process of other vaccines, saying, “I have researched the development process of other vaccines (he was holding a paper in his hand). For example, the rabies vaccine took four years to develop, tetanus took 40 years, diphtheria 40 years, and meningitis eight years. How is it possible that the COVID-19 vaccines were developed in just one year?” (Distrust of vaccine companies).
Perceived Benefits
In the analysis of in-depth interviews, we identified two different perceived benefits as “protecting themselves from side effects” and “feeling more dignified” (Table 1). Regarding the aspect of protecting themselves from side effects, one HCW (P5) expressed, “I have seen some cases of cerebrovascular accidents after the COVID-19 vaccines. I also heard about this from my close friends. Although scientists have tried to prevent these cases, they have not been successful. I have witnessed numerous instances involving my close relatives that demonstrate the devastating side effects of the COVID-19 vaccines.” Another HCW (P9) mentioned, “I have observed many adverse experiences related to the COVID-19 vaccines. I had a friend who was a pediatric surgeon. He had a heart attack after the second COVID-19 shot. His wife, a cardiology specialist, stated that his echocardiography was perfect just six months prior.”
Perceived Self-Efficacy
Under the self-efficacy component, we identified five different codes (46 statements) supporting vaccine hesitancy among HCWs. The most common codes among vaccine-hesitant HCWs were “trust their self-immunity” and “strictly compliance with pandemic rules”. One HCW P12) expressed their reasoning for not getting vaccinated, stating, “I was not vaccinated because I trusted my immune system cognitively, psychologically, and physiologically. I believed that I was ready to handle the disease. I take vitamin supplements from time to time, and I cannot do sports. I believe in the power of thought and practice affirmative thinking. I love my body, and I have a good relationship with my organs. I do not interfere with my organs, and we are like friends. I believe that all these factors contributed to my decision not to be vaccinated.”
Perceived Severity and Susceptibility (Perceived Threat)
Vaccine-hesitant HCWs reported 15 different perceived severity and susceptibility sub-theme codes related to COVID-19 vaccine hesitancy. These codes were categorized into five sub-themes: immunity, self-protection from external factors, self-protection from vaccine side effects, feeling at risk or not, and protection from vaccine and pharmaceutical companies (55 statements), side effects (42 statements), and vaccination and therapy processes (37 statements) were the most common theme codes. The sub-theme of protecting oneself from side effects was also linked to perceived benefits. Some HCWs viewed COVID-19 as a risk to their health, while others did not believe their health was at risk. We collected 14 expressions that supported non-pharmaceutical intervention, while only two expressions contradicted non-pharmaceutical intervention during the pandemic.
Cues to Action
One of the questions in the semi-structured interview forms was, “What kind of regulation or arrangement could persuade you to get the COVID-19 vaccine?”. The responses from participants were categorized into four different titles: personal, management, vaccine, and disease-related regulations or arrangements. The most common persuasive factors were related to the COVID-19 vaccines themselves. Participants stated that if the vaccines were “more effective” (10 statements) or “did not require booster doses” (9 statements), they would be more willing to get vaccinated. One HCW expressed their sentiment, saying, “If people had not died after COVID-19 vaccination if the vaccine could protect people from the disease, I would gladly get vaccinated.” Another HCW mentioned, “The COVID-19 vaccine still does not protect people. If it had the same level of protection as the Hepatitis B vaccine, I might consider getting it.” Conversely, we identified nine different statements suggesting that HCWs might be more willing to get vaccinated if the vaccine had no side effects and, unlike other vaccines, had not been developed so quickly. For example, one participant (G1) expressed her viewpoint, saying, “If the pandemic had been managed properly, if the restrictions such as lockdowns and mask rules had been consistently enforced from the beginning, if the COVID-19 disease therapy process had been handled appropriately and consistently, I would willingly get vaccinated like others.”
Discussion
This study aimed to understand better vaccine hesitancy among HCWs during the pandemic. In-depth interviews based on the HBM were conducted with vaccine-hesitant HCWs. A total of 790 different expressions provided by these vaccine-hesitant HCWs were analyzed.
There are several studies have demonstrated a link between perceived barriers and vaccine hesitancy (19, 20). Indeed, the analysis of interviews with vaccine-hesitant HCWs revealed that perceived barriers to COVID-19 vaccination fell into six main categories: distrust, fear of uncertainty, immune confidence and spirituality, the media effect, social pressure, and obstinacy. Among these, the three most prevalent reasons for vaccine hesitancy were consistent with existing literature: conflicting news about COVID-19 vaccines, fear of unexpected vaccine side effects, and lack of trust in pharmaceutical or vaccine companies (10, 13, 15).
Another noteworthy factor contributing to vaccine hesitancy among HCWs was related to governance. Some HCWs expressed a lack of trust in the advice provided by their country’s Ministry of Health. This lack of trust in government guidance and recommendations has been shown in a systematic review study conducted by Wang et al., where trust in the government was identified as a strong predictor of COVID-19 vaccination willingness (24). Moreover, some vaccine-hesitant HCWs stated that they were pressured by family members, physicians, or close friends not to receive any COVID-19 vaccine. As supported by the cross-sectional study conducted by Li et al., family or doctor’s advice can be the most critical factor affecting people’s future vaccination intentions (21). Similarly, another study conducted with HCWs demonstrated that 66% of HCWs reported a willingness to get vaccinated if their colleagues or friends were also vaccinated (n=1680) (25). Therefore, positive vaccination attitudes within the immediate circle play a crucial role in increasing the vaccination rate among HCWs.
Some participants admitted to subscribing to conspiracy theories, while others displayed confidence in their own immune system’s ability to protect them. Interestingly, some HCWs believed that an unjustified, deep fear of the pandemic or death was deliberately instigated by unidentified entities or even questioned the existence of the pandemic or the SARS-CoV-2 virus itself. Additionally, certain HCWs cited the need for booster doses as a reason for their vaccine hesitancy. These unique perspectives shed light on the diverse range of factors influencing vaccine hesitancy among HCWs and highlight the importance of understanding individual beliefs and attitudes in carrying out effective vaccination campaigns.
Media can be a source of rapid communication or misinformation, which may contribute to negative attitudes due to easy and inexpensive access for many users. So, the impact of media should not be underestimated when assessing vaccine hesitancy, as some HCWs attributed their reluctance to information they encountered on social media or traditional media outlets like television programs, magazines, or news articles.
We also identified other distinct reasons for vaccine hesitancy among HCWs. Fear of unforeseen side effects appears to be a deterrent for some HCWs, leading to vaccine hesitancy. On the other hand, for some vaccine-hesitant HCWs, this fear might be perceived as a benefit, as it reinforces their decision not to get vaccinated. Additionally, some HCWs expressed a desire to differentiate themselves from others or resist joining the majority, who were quickly convinced and vaccinated. Their statements, such as “If others can get the vaccine easily, I become suspicious” and “I am different from others; these activities cannot persuade me,” suggest that they were reluctant to conform to societal norms and identified more closely with a minority group of vaccine-hesitant individuals. Maciuszek et al. emphasized the significance of group identities in shaping vaccination decisions, not only for pro-vaccine individuals but also for those who are hesitant about vaccines (26). Similarly, Dr. Renn described this phenomenon as “the sense of belonging within a community of like-minded people” (27). Consequently, vaccine-hesitant HCWs may maintain their positions and hesitancy to support and identify with others who share similar views. Addressing vaccine hesitancy among HCWs should take into account the role of social dynamics and group influences. Strategies aimed at increasing vaccination rates should not only provide accurate information about the vaccines’ safety and efficacy but also consider the psychological and social factors that shape individuals’ decisions.
In the in-depth interview analysis, vaccine-hesitant HCWs proposed various regulations and suggestions related to COVID-19 vaccination, which were categorized into four themes: personal, management, vaccine, and disease-related regulations or arrangements. The most common recommendation focused on the COVID-19 vaccines themselves. HCWs expressed the need for vaccines that offer complete protection from the disease, do not require booster doses, have fewer unexpected side effects, and undergo a thorough and non-hurried development process. These suggestions highlight the importance of addressing HCWs’ concerns and preferences when designing vaccination programs and campaigns. HCWs’ recommendations reflect their desire for vaccines that are not only highly effective but also perceived as safe and trustworthy. Concerns about vaccine effectiveness, side effects, and the development process may be significant barriers to vaccination among HCWs, as reported in the study by Al-Metwali et al. (25).
Management-related suggestions were also prominent among vaccine-hesitant HCWs. They expressed that making COVID-19 vaccination mandatory, improving and consistent pandemic management, reducing pressure to get vaccinated, and increasing access to comprehensive vaccine information would encourage them to consider vaccination. On the other hand, in the previous study, we found that some nudging interventions, such as mandatory PCR tests and education, were effective approaches to increasing vaccination. However, in this study, we interviewed employees who continued not to get vaccinated despite all prodding attempts, and their reactions were different from those of previous employees. This statement is proof that not all nudge interventions will be 100% effective on all HCWs who are hesitant about vaccination. Additionally, vaccine-hesitant HCWs desired greater transparency from the government regarding case numbers and pandemic-related data. Implementing these suggestions could be crucial role in addressing vaccine hesitancy among HCWs.
During the interviews with vaccine-hesitant HCWs, some mentioned personal factors influencing their decision, such as considering vaccination if they had comorbidities or had experienced the loss of a relative to COVID-19. Others suggested that a higher disease-related mortality rate might motivate them to get the COVID-19 vaccine. Interestingly, Al-Metwali et al. reported that a significant percentage of HCWs (26.2%) did not perceive a high risk of infection during the pandemic, and 24% of HCWs did not believe that COVID-19 was a fatal disease. These differing perceptions of risk and severity may contribute to vaccine hesitancy among HCWs and underscore the importance of personalized communication and education strategies to address their concerns effectively (25). The perceived risk and safety perceptions are complex and may vary among individuals based on their experiences, beliefs, and understanding of the pandemic. Addressing these concerns and providing accurate information about vaccine safety and efficacy remains crucial to promoting vaccination among vaccine-hesitant HCWs.
The insightful suggestions from vaccine-hesitant HCWs indicate the importance of not assuming HCWs are well-informed about vaccines during pandemics. Re-education is needed on pandemic vaccines, emphasizing their benefits, low side effect risk, booster dose advantages, and rigorous development process. Authorities should use transparent and detailed information dissemination methods to address HCWs’ concerns. Furthermore, the possibility of mandatory vaccination for HCWs during pandemics should be carefully considered, balancing individual rights and ethics. Open dialogue and respectful consideration of HCWs’ concerns are vital to combat vaccine hesitancy and ensure safety for all during pandemics.
This study has some limitations that should be acknowledged. Firstly, the qualitative nature of the methodology limits generalizability to all HCWs, but it provides valuable in-depth insights into vaccine hesitancy among this group. Future studies could aim for broader samples to enhance generalizability. Secondly, the study’s sample was confined to two hospitals within the same consortium, potentially affecting the representation of HCWs’ opinions in other regions with different institutional cultures. Thirdly, the high vaccination rate in our hospitals may have limited the number of vaccine-hesitant HCWs, potentially making their reactions more pronounced compared to the general population of vaccine-hesitant HCWs. Despite these limitations, the study’s strengths lie in its qualitative approach, offering unique perspectives and unexplored insights to researchers and authorities managing pandemics.
HCWs play a crucial role in the pandemic response, making their vaccination decisions particularly significant. Vaccine hesitancy among HCWs should not be overlooked, and understanding the underlying factors is essential for increasing vaccination rates. Utilizing the HBM and qualitative research methods, we have gained valuable insights into the reasons behind vaccine hesitancy among HCWs. These detailed findings can guide future vaccination campaigns during pandemics and contribute to improving overall vaccination rates among HCWs. Recognizing and addressing the concerns of HCWs will ultimately lead to better protection for themselves, their close circles, and the communities they serve.