Introduction
Healthcare-associated infections (HAIs) are common yet largely preventable through adherence to evidence-based guidelines. In 2005, Türkiye implemented a national infection control program, which led to significant reductions in HAI rates, including a 50% decrease in central line-associated bloodstream infections (CLABSIs) between 2008 and 2017 (1). This result was in parallel with data from the U.S. Centers for Disease Control and Prevention (CDC) National Healthcare Safety Network (NHSN), which also showed significant progress in HAI prevention (2).
However, the coronavirus disease 2019 (COVID-19) pandemic disrupted infection control practices in healthcare settings worldwide. In particular, the rapid surge in critically ill patients overwhelmed hospital capacities, making it difficult to sustain proper infection control protocols (3). Multiple studies have reported increased CLABSI rates during the pandemic, particularly in its early phases and at the height of COVID-19 prevalence (4-10).
Central line-associated bloodstream infections are a significant ongoing problem, contributing to increased mortality, morbidity, prolonged hospital stay, and higher healthcare costs. Understanding the impact of the COVID-19 pandemic on CLABSI rates may help inform infection prevention priorities and guide future preparedness efforts in the event of new epidemics or pandemics. In this study, we aimed to evaluate the impact of the COVID-19 pandemic on CLABSI in Türkiye, a country with one of the highest antibiotic resistance rates among Organisation for Economic Co-operation and Development (OECD) member states, over a four-year period from 2019 to 2022 (11).
Materials and Methods
Study Population
This retrospective, multicenter study included 25 hospitals in Türkiye, categorized by bed capacity as follows: 150–500 beds (n=11), 500–1000 beds (n=10), and >1000 beds (n=4). At least one center from each geographical region in Türkiye participated: Marmara Region (n=11), Central Anatolia Region (n=4), Black Sea Region (n=3), Aegean Region (n=3), Eastern Anatolia Region (n=2), Southeastern Anatolia Region (n=1), and Mediterranean Region (n=1). All hospitalized patients diagnosed with CLABSI according to the NHSN criteria of the CDC, between January 2019 and December 2022, were included.
Study Design
A retrospective analysis was conducted using prospectively collected CLABSI data from routine surveillance over a four-year period. The study timeline was divided into three intervals: the pre-pandemic period (January 1, 2019–March 10, 2020), the early pandemic period (March 11, 2020–December 31, 2021), and the late pandemic period (January 1, 2022–December 31, 2022).
Demographic and clinical characteristics of the study population, as well as CLABSI-related fatality rates, were analyzed. Microorganism distributions and antibiotic resistance rates were compared between the pre-pandemic and pandemic periods. Additionally, trends in resistance rates of multidrug-resistant (MDR) pathogens were examined across the same time intervals.
Definitions
In Türkiye, nationwide prospective, patient-based, and active surveillance of HAIs and their causative microorganisms is mandatory in all intensive care units and optionally in general wards. Surveillance definitions are standardized and aligned with CDC NHSN criteria (12,13). Central line-associated bloodstream infection was defined as a positive blood culture in a patient who had a central line in place within 48 hours prior to the onset of bloodstream infection, not attributable to another infection site.
Microorganisms were identified using automated systems routinely used in each center. Antibiotic susceptibility was assessed via disc diffusion or minimum inhibitory concentration testing, and results were interpreted according to the European Committee on Antimicrobial Susceptibility Testing (EUCAST) guidelines (14). Multidrug-resistant pathogens were defined as those exhibiting acquired resistance to at least one agent in three or more antimicrobial categories (15). According to the World Health Organization (WHO) classification, Acinetobacter spp., Pseudomonas spp., and Enterobacteriaceae are critical and high-priority MDR pathogens due to the urgent need for new antibiotics (16).
Statistical Analysis
Statistical analyses were performed using Student’s t-test for comparisons between two groups and one-way analysis of variance (ANOVA) for comparisons among more than two groups for continuous variables. The chi-square test was used for categorical variables. The normality of distribution was assessed using the Shapiro-Wilk test. For non-normally distributed continuous variables, the Mann-Whitney U test (for two groups) and the Kruskal-Wallis test (for more than two groups) were applied. Pearson’s correlation coefficient was used to analyze the relationship between CLABSI rates and catheter utilization rates.
Time series analysis was performed to show trends in CLABSI and catheter utilization rates throughout the study period. All analyses were performed using STATA software (version 15, StataCorp, College Station, TX, USA), with statistical significance set at p<0.05.
Results
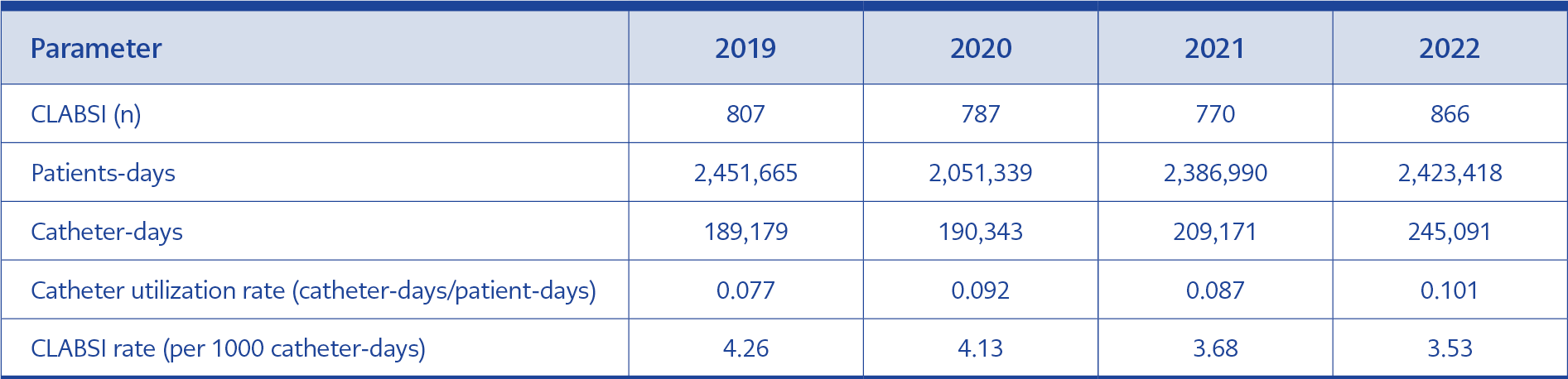
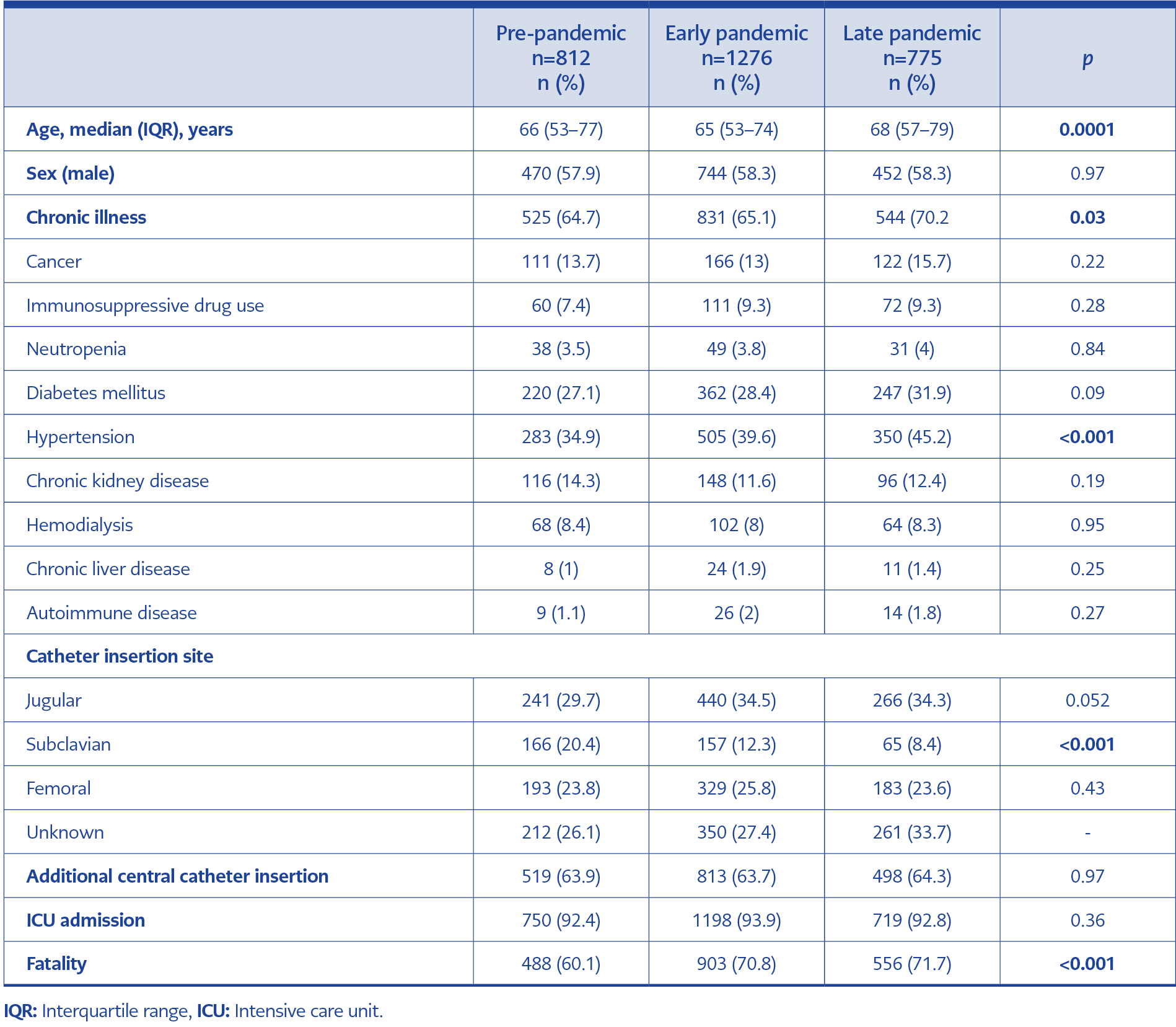
Table 1. Demographic characteristics, clinical signs and symptoms, and surgical procedures in patients with COVID-19-associated mucormycosis (CAM) (n=28).
Central line–associated bloodstream infection rates per 1000 catheter days were 4.26 in 2019, 4.13 in 2020, 3.68 in 2021, and 3.53 in 2022. Catheter utilization and CLABSI rates by year are presented in Table 1. There was no significant correlation between CLABSI and catheter utilization rates (Pearson’s r = –0.725; p=0.275).
A total of 2863 CLABSI cases were included in the study, of which 2666 (93%) occurred in intensive care units (ICUs). Of these, 28.4% occurred during the pre-pandemic period, 44.6% during the early pandemic, and 27% during the late pandemic period. Time series analysis revealed a statistically significant decrease in CLABSI rates over the study period (multiple R²=0.9475; adjusted R²= 0.9212; F (1, 2)=36.07; p=0.027). However, the change in catheter utilization rates was not statistically significant (multiple R²=0.7463; adjusted R²=0.6195. F(1, 2)=5.883; p=0.136).
The gender distribution of patients with CLABSI was consistent across the three periods: 470 of 812 (57.9%) in the pre-pandemic period, 744 of 1276 (58.3%) in the early pandemic period, and 452 of 775 (58.3%) in the late pandemic period (p=0.97). The median age of the patients was 66 years during the pre-pandemic period, 65 years during the early pandemic, and 68 years during the late pandemic (p=0.0001). A total of 392 patients had been diagnosed with COVID-19 within 30 days prior to their CLABSI diagnosis, and 321 of these had a positive severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) PCR test. Hospital mortality rates increased from 60.1% the pre-pandemic period to 70.8% and 71.7% in the early and late pandemic periods, respectively (Table 2).
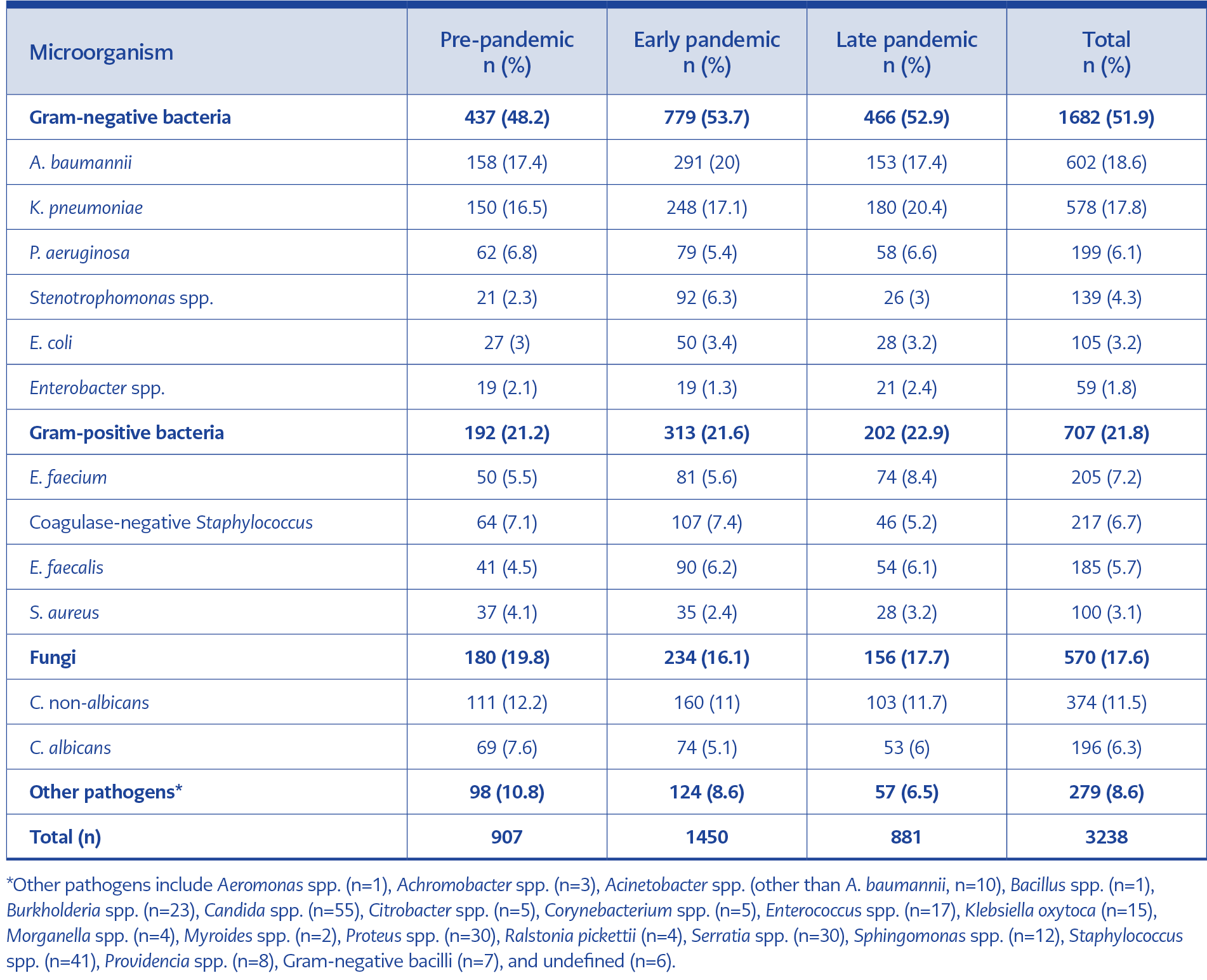
Table 3. Distribution of pathogens isolated from patients with central line-associated bloodstream infection (CLABSI) by study period.
In total, 3238 pathogens were identified. Gram-negative bacteria were the most common pathogens in both the pre-pandemic and pandemic periods. The most prevalent pathogens were A. baumannii (18.6%), K. pneumoniae (17.8%), and Candida non-albicans (11.5%). Among Gram-positive organisms, methicillin-resistant coagulase-negative staphylococci (MRCoNS) were most common in the pre-pandemic and early pandemic periods, while Enterococcus faecium predominated in the late pandemic period. The other pathogens are presented in Table 3.
Although quinolone resistance in Gram-negative pathogens showed a continuous upward trend, the change was not statistically significant (p=0.2). A. baumannii exhibited the highest carbapenem resistance, increasing from 94% to 97%. Notably, K. pneumonia showed a significant increase in resistance to both carbapenems (p=0.015) and colistin (p=0.004) during the pandemic periods compared to the pre-pandemic period. Changes in colistin resistance in Escherichia coli (p=0.39) and P. aeruginosa (p=0.1) were not statistically significant.
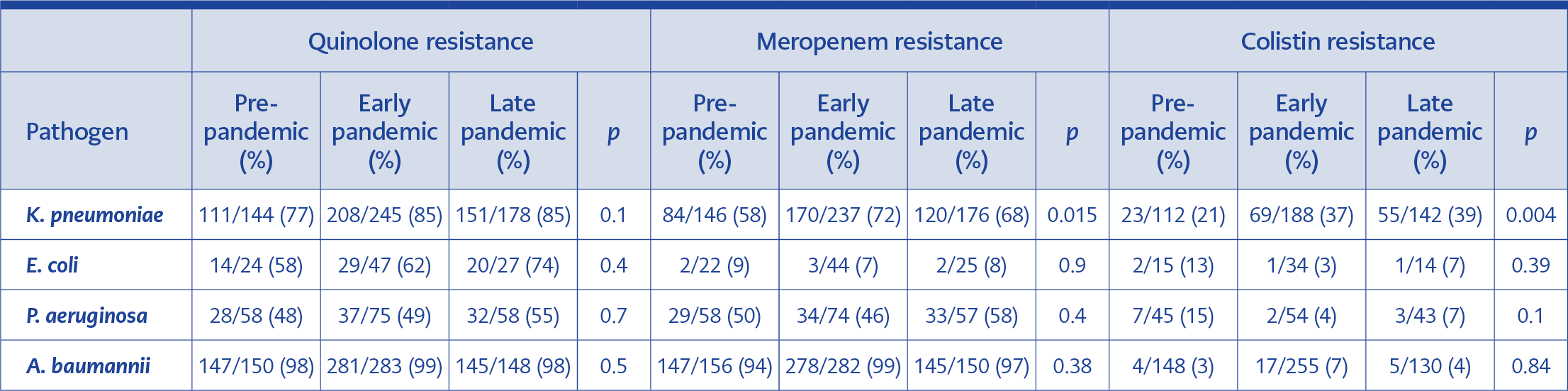
Table 4. Antibiotic resistance rates of selected pathogens causing central line-associated bloodstream infection (CLABSI) in the pre-pandemic and pandemic periods.
Ceftazidime-avibactam resistance in K. pneumoniae also increased during the pandemic, and resistance was detected in 33% of P. aeruginosa isolates. The changes in antibiotic resistance rates of pathogens between the pre-pandemic and pandemic periods are summarized in Table 4.
Discussion
The surge in critically ill patients in ICUs during the COVID-19 pandemic had a detrimental effect on essential infection control practices within healthcare institutions. Several factors contributed to the rise in healthcare-associated infections, including the restructuring of hospitals to accommodate increasing admissions, heightened workloads for healthcare workers, the use of immunomodulatory treatments in COVID-19 patients, and prolonged catheter use.
Studies from various countries have demonstrated that CLABSI showed the most significant increase among HAIs during the pandemic (4-10). In our multicenter study, which included four years of data from 25 hospitals across TÜrkiye, 44.6% of all CLABSI cases occurred during the early pandemic period. However, unlike many international reports, we did not observe an overall increase in CLABSI rates during the pandemic in Türkiye.
One potential reason for the stable CLABSI rates is the disruption of routine surveillance practices, particularly during the early stages of the pandemic. Central line-associated bloodstream infection cases may have been underdiagnosed due to hesitancy in obtaining blood cultures—especially during periods of patient surges—and because bacteremia in patients with COVID-19 pneumonia often did not meet standardized diagnostic surveillance criteria.
This finding contrasts with other studies. For instance, a seven-country evaluation examining the impact of COVID-19 on HAIs in ICUs reported an 85% increase in CLABSI rates during the pandemic’s first year compared to 2019 (17). Similarly, national data from the United States indicated significant increases in HAI rates during the first year of the pandemic, with CLABSI showing the most pronounced rise (10). A global review assessing the impact of COVID-19 on CLABSI revealed that 17 out of 21 studies reported a significant increase in CLABSI incidence and rates during the pandemic (18).
Recurrent risk factors identified in previous studies, such as increased workloads, the redeployment of staff, and overwhelmed healthcare personnel, negatively impacted essential infection control practices and likely contributed to the globally increased CLABSI rates during the pandemic. In contrast, the absence of a marked increase in CLABSI rates in our study may be partly explained by the heterogeneity of the participating centers. Several of the hospitals included were state institutions with lower patient volumes, and many experienced significant decreases in hospital admissions during the peak phases of the pandemic.
Studies conducted during the pandemic period indicate that CLABSI developed more readily in patients infected with SARS-CoV-2. One study from Türkiye demonstrated that, despite shorter lengths of stay in COVID-19 ICUs, CLABSI rates were higher compared to general ICUs, with infections developing more quickly in patients with COVID-19 (19). Central line-associated bloodstream infection significantly increases patient morbidity and mortality. A multinational study comparing CLABSI outcomes between critically ill patients with ot without COVID-19 found that those with SARS-CoV-2 were more susceptible to CLABSI and had significantly higher mortality rates (58.7% vs 40%) (20). In line with these findings, our study observed an increase in CLABSI-related mortality during both the early and late pandemic periods compared to the pre-pandemic period.
In TÜrkiye, the distribution of CLABSI pathogens remained predominantly Gram-negative during the pandemic, with A. baumannii and K. pneumoniae being the most frequently identified pathogens (19,21,22). In contrast, some studies reported a predominance of Gram-positive bacteria, particularly Enterococcus species and coagulase-negative staphylococci, during the pandemic period (20,23-25). The pandemic also significantly impacted global patterns of antibiotic resistance. Our findings demonstrated a notably high and increasing rate of colistin resistance in K. pneumoniae, along with rising trend in carbapenem resistance. A systematic review of studies published from December 2019 to May 2022 reported colistin resistance rates during the pandemic period as 2.5% for A. baumannii, 21.1% for K. pneumoniae, and 4% for P. aeruginosa (26). In comparison, our study found higher colistin resistance among K. pneumoniae isolates, with resistance continuing to rise following the pandemic. In Türkiye, Ergönül et al. (27) reported a colistin resistance rate of 6% in K. pneumoniae in 2013, whereas our study documented a rate of 39% in 2022. Similarly, carbapenem resistance in K. pneumoniae increased sharply, from 38% in 2013 to 68% in 2022.
Our study has several limitations. Firstly, in addition to hospitals that managed COVID-19 patients during the pandemic, state hospitals not designated as pandemic centers were also included. Second, because of its retrospective design, data on patients’ baseline clinical severity, prognostic scores, and antimicrobial treatment regimens were not available. Third, CLABSI rates were not compared separately for wards and ICUs, which may introduce variability due to heterogeneity in care settings. Finally, our findings could not be directly compared with national surveillance data, which are reported annually and stratified by ICU type, whereas our study was based on pandemic phases.
In conclusion, this multicenter study demostrated that CLABSI rates in Türkiye decreased from 4.26 to 3.53 per 1000 catheter days between 2019 and 2022, contrary to global trends that reported increases during the COVID-19 pandemic. Gram-negative bacteria—notably A. baumannii (18.6%) and K. pneumoniae (17.8%)—remained the most common pathogens. A significant increase in antimicrobial resistance was observed, especially for carbapenems (68%) and colistin (39%) in K. pneumoniae, compared to pre-pandemic levels. Additionally, hospital mortality linked to CLABSI increased from 60.1% pre-pandemic to 71.7% in the late pandemic period. These findings underscore the importance of sustained infection prevention efforts and antimicrobial stewardship, particularly during disruptions to the healthcare system, such as pandemics.