Introduction
Staphylococcus aureus colonizes the skin and mucosa of humans. Infections because of S. aureus can range from skin infections to potentially fatal conditions like pneumonia, sepsis, and endocarditis. S. aureus is a common cause of nosocomial and community-acquired bloodstream infections worldwide (1). Because of biofilm development, it is also one of the causes of long-term and complex treatments in prosthetic implants and central-line catheters (2). The clinical approach to S. aureus bacteremia (SAB) includes a detailed history and physical examination, infectious disease specialist consultation, repetitive blood culture, focus detection, and diagnostic evaluation, including echocardiography and additional imaging as needed (3).
Previous studies have investigated the impact of structured interventions on SAB management and identified some quality indicators with promising outcomes (4). Some of these studies have reported a decrease in 30-day mortality, with rates falling below 10% after improving compliance with quality indicators (5). However, despite appropriate treatment and early diagnosis methods, the mortality rate in SAB has ranged from 10% to 30% in recent years (6).
This study aims to evaluate the clinical features and approaches to SAB in a tertiary care center and to analyze the parameters that may affect 7-day and 30-day mortality.
Materials and Methods
Setting and Study Population
We performed this at Başkent University Hospital between January 01, 2011, and July 01, 2018. Başkent University Hospital is a 350-bed tertiary-care center with approximately 48,000 admissions monthly. The positive blood culture for S. aureus was confirmed retrospectively via the review of the bacteriology laboratory. Adult patients (≥18 years) who were defined as positive for S. aureus based on at least one blood culture by the infectious diseases (ID) specialist and followed at least one month after the initiation of treatment were included in the study. In organizing the study, the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) rules were followed (7).
Data Collection
Clinical data, patient demographics, and 7-day and 30-day mortality rates were obtained using electronic medical records. Death within seven days following the index blood culture was defined as 7-day mortality and death within 30 days as 30-day mortality. Patient demographics and comorbidities included age, gender, presence of immunosuppression, malignancy, chronic heart disease, chronic renal disease, and diabetes mellitus. Cardiac devices included a left ventricular assist device, pacemaker, and previous valve replacement.
An infectious disease specialist, using a standardized form, collected the data on the infectious focus, consultation with an ID specialist within 96 hours of the index blood culture, echocardiography, fundoscopic examination, imaging (abdominal computed tomography [CT], head computed tomography), adequacy and timing of antibiotic treatment, the length of hospital and intensive care unit (ICU) stay. Re-infections were excluded; only the last episode was included in the study. Patients were followed for one month after the index blood culture.
Infective Focus Definitions
In addition to some unknown sources, SAB episodes were caused by endocarditis, osteoarticular, intraabdominal, respiratory, and central catheter-related infections. The source of SAB was determined by isolating similar S. aureus strains from blood and the drainage of particular samples, such as sputum and pus, which were obtained from body sites compatible with clinical or radiological signs of infection. Endocarditis was defined according to modified Duke criteria. The Infectious Diseases Society of America (IDSA) Guideline was used to define central catheter-related bloodstream infection (8).
Microbiological Studies
Blood cultures were processed in the laboratory using BD BACTEC™ FX automated system (Becton Dickinson, NJ, USA). When growth occurred, it was gram-stained and inoculated on sheep blood medium and eosin methylene blue medium at 370C for 24 to 48 hours. Bacterial identification of S. aureus was based on gram stain, positive tube coagulase, and mannitol reaction. Antimicrobial susceptibility was performed on BD Phoenix™ (Becton Dickinson, NJ, USA). In addition, the disk diffusion susceptibility test was used, while the antibiotics included cefoxitin, rifampicin, erythromycin, and clindamycin.
Antibiotic Treatment
For methicillin-susceptible S. aureus (MSSA), the initiation of empirical beta-lactam, glycopeptide, and daptomycin was considered appropriate; cefazolin was defined to be appropriate for maintenance therapy. Using glycopeptide, linezolid, and daptomycin as empirical and maintenance therapy for methicillin resistant S. aureus (MRSA) was considered appropriate.
Statistical Analysis
The statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) 26.0 program (IBM Corp., Armonk, NY, USA). Continuous variables are presented by mean±SD and median (minimum-maximum) values, whereas categorical variables are represented by number and percentage distributions. The Chi-Square and Fisher’s exact tests were used for categorical variables to assess mortality in the first seven days and 30 days. The Kolmogorov-Smirnov and Mann-Whitney U tests were used to assess conformity to the normal distribution of continuous variables. The statistical significance was set as p<0.05. Binary logistic regression analysis was performed by designing the model with factors associated with 7-day and 30-day mortality in univariate analyses. The model’s suitability was evaluated with the Hosmer-Lemeshov test, and the entered model was used in logistic regression analysis.
Results
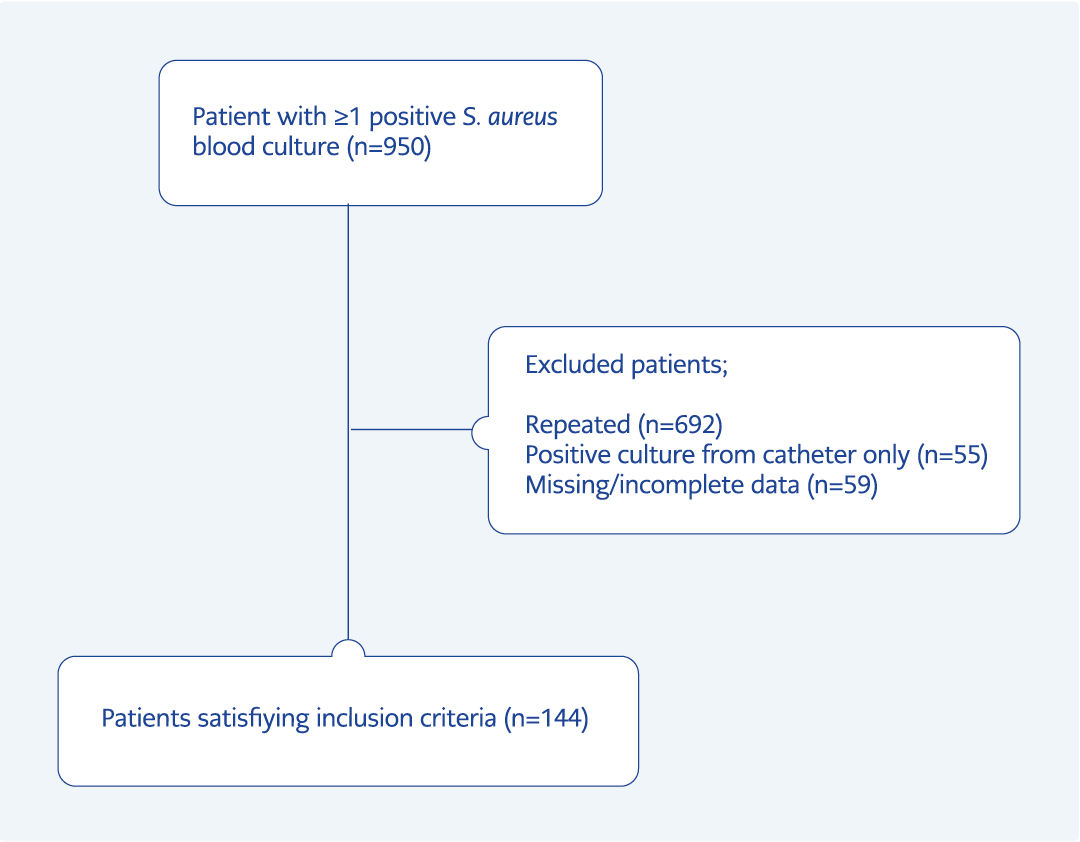
There were 950 results with S. aureus isolation in the blood culture in the relevant period; 692 repeated results from the same patients, 55 results from only the catheter, and 59 patients with incomplete or missing medical records were excluded (Figure 1). A total of 144 bacteremia episodes were included in the study. Eighty-three (57%) patients were men. The mean age was 65.2±16.5 years, and 57.6% (83/144) patients were ≥65 years old.
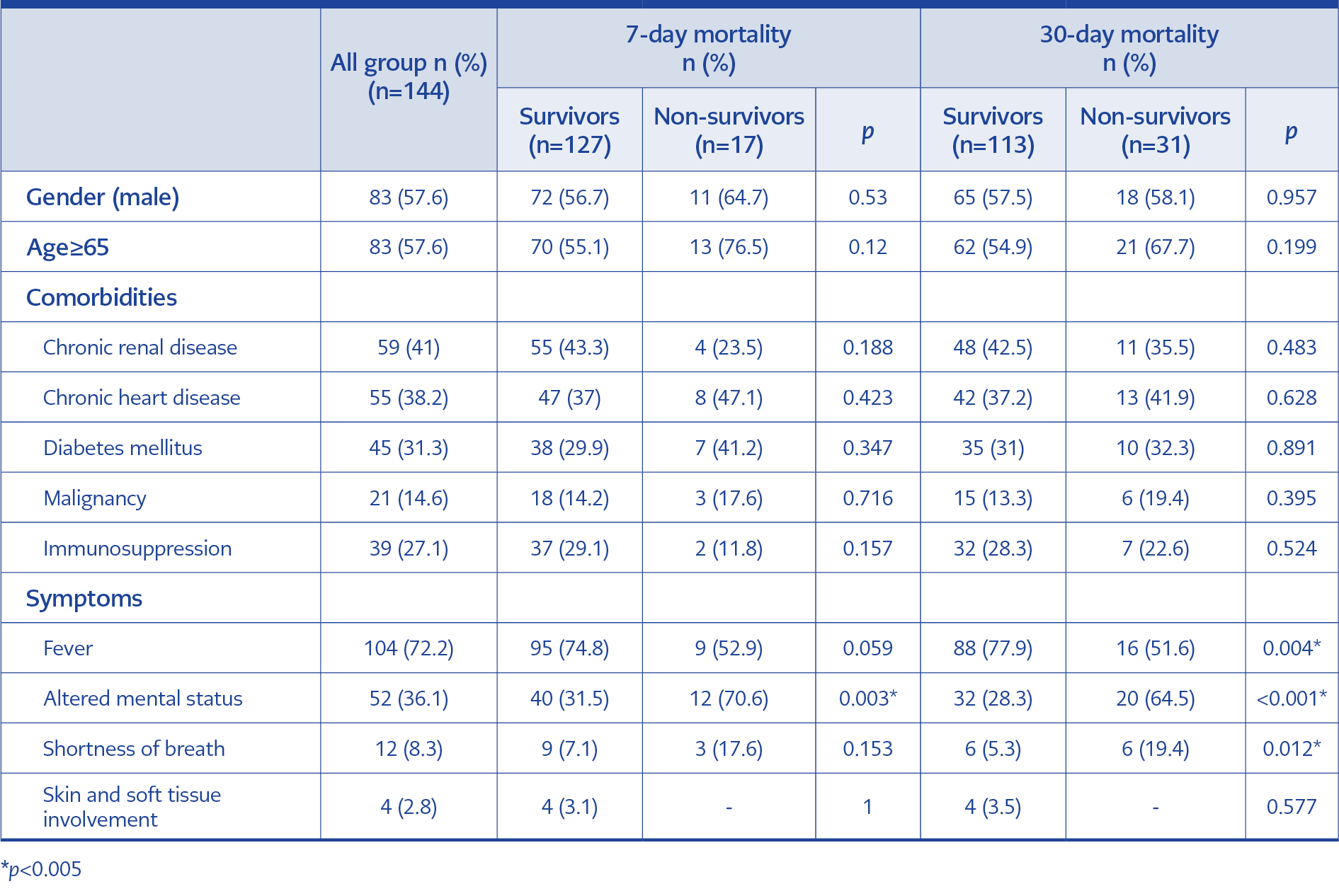
The most common comorbidities were chronic renal failure 41% (59/144), followed by chronic heart disease 38% (55/144), and diabetes mellitus 31% (45/144). The most common admission symptom was a fever of 72%. The other admission symptoms were altered mental status (36%), shortness of breath (8%), and skin and soft tissue signs (2%). The demographic characteristics of patients are shown in Table 1.
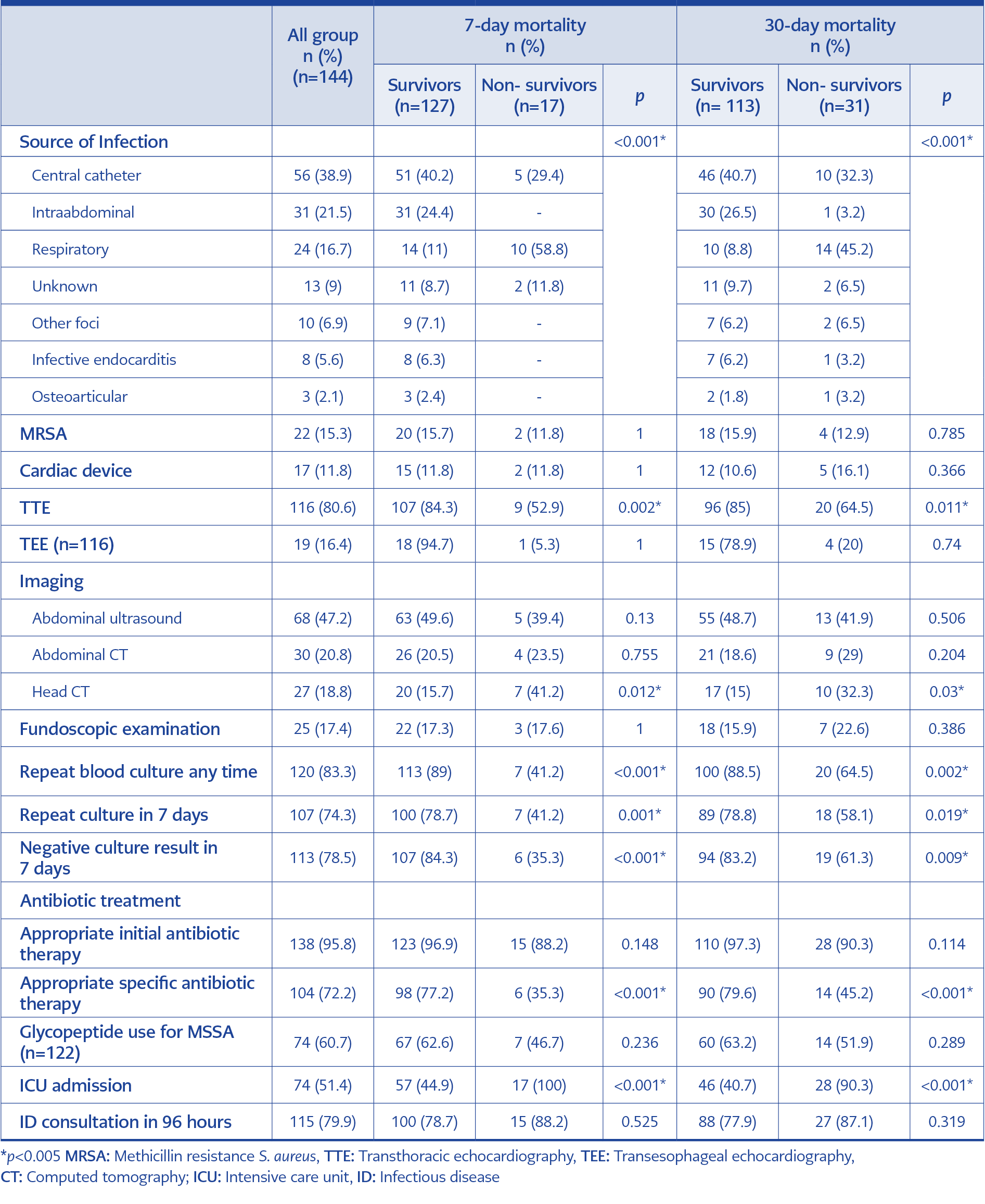
The primary sources of infection were central-line catheter (38.9%), intraabdominal (21%), respiratory (16.7%), infective endocarditis (5.6%), and osteoarticular (2.1%). Thirteen of 24 patients with a respiratory focus were diagnosed radiologically, eight with respiratory tract specimens S. aureus isolation, and three both radiologically and with respiratory tract specimens. Fifteen of 31 patients with intraabdominal focus had a concurrent intraabdominal infection (such as abscess, cholangitis, or peritonitis), ten had SAB that developed within 48 hours of an invasive procedure or surgery, and six had active abdominal malignancy.
MSSA strains were more commonly isolated than MRSA (84.7%, and 15.3%, respectively). Transthoracic echocardiography (TTE) was performed at 80.6% (116/144) of patients with a high rate. Transesophageal echocardiography (TEE) was needed in only ten patients. TTE was performed significantly lower in the non-survivor group than in the survivor group (p=0.002; p=0.011, respectively). The most common abdominal imaging method was an ultrasound, but only 47.2% of patients were examined. Only 17.4% of patients had a fundoscopic examination.
We obtained repeat blood cultures from 83.3% (120/144) of patients, and 74.3% (107/144) of patients’ blood cultures were obtained within seven days. The number of patients with negative results within seven days after the index blood culture was 78.5% (113/144). The decrease in the rate of repeat blood cultures in 7 days to 41.2% in the 7-day mortality group was because the patients were lost in a shorter period. Appropriate antibiotic therapy was initiated in 95.8% of the patients. However, the maintenance treatment was deemed appropriate at 72.2% (104/144). The main reason for inappropriate maintenance therapy was the initial treatment (broad-spectrum antibiotics such as carbapenem, teicoplanin, piperacillin-tazobactam, linezolid, or combination therapies) was continued even though the causative agent was MSSA in critically ill patients.
Repeat blood culture any time during hospitalization, repeat blood culture in 7 days, and negativity control in 7 days were found to be significantly high in survivors (in 7-day mortality group: p<0.001, p=0.001, p<0.001, respectively; in 30-day mortality group: p=0.002, p=0.019, p=0.009, respectively).
ID specialist consultation was requested in 79.9% of the patients within 96 hours following the index blood culture signal. ID consultation was high as %75 in all groups and reported no correlation with mortality.
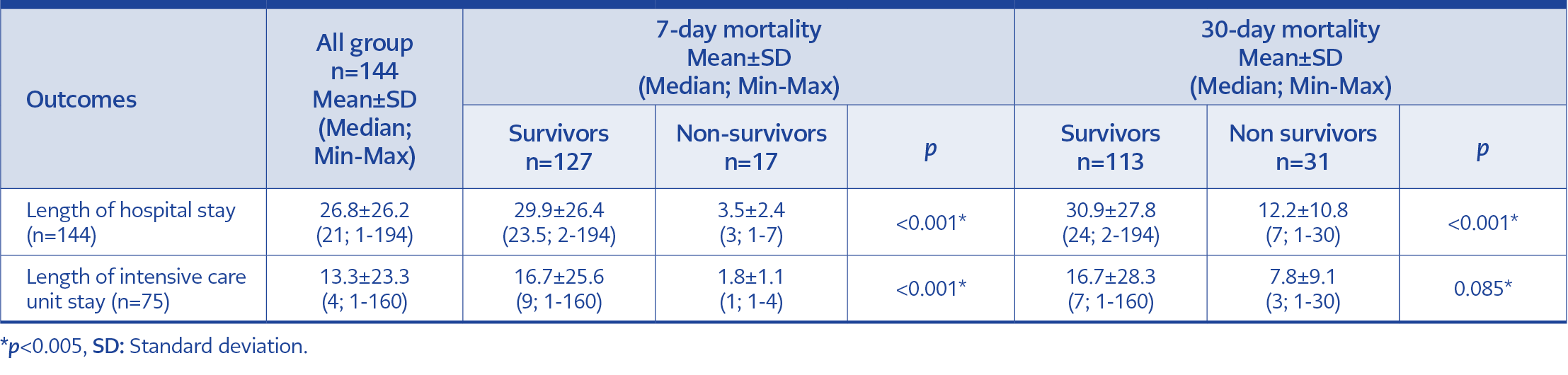
Overall 7-day mortality was 11.8% (17/144), and 30-day mortality was 21.5% (31/144). Altered mental status at admission was associated with higher mortality (p=0.003 in the 7-day mortality group and p<0.001 in the 30-day mortality group). As a result, head CT performed higher in non-survivor groups. The patient with a respiratory focus had a significantly high mortality rate (58.8% in the 7-day mortality group and 45.2% in the 30-day mortality group). The clinical approach and outcomes of patients with SAB are shown in Table 2. The median length of hospital stay in all groups was 21 days (min=1 – max=194), and the intensive care unit stay was 4 days (min=1 – max=160). The length of stay is detailed in Table 3.
In univariate analysis, there was a correlation between 7-day mortality and altered mental status, a respiratory focus, echocardiography imaging, ICU admission, head CT, any time repeat blood culture, repeat blood culture in 7 days, negative blood culture result in 7 days, and appropriate specific therapy. However, multivariate analysis did not identify any factors that could affect mortality. On the other hand, 30-day mortality increased with ICU admission and the presence of a respiratory focus. ICU admission increased the risk of 30-day mortality by 1.12 times (odds ratio [OR]=1.123; 95% confidence interval [CI]=2.506-5.000); the presence of a respiratory focus increased the risk by 4.36 times (OR=4.366; 95% CI=1.223-15.625). There was no relationship between other variables and 30-day mortality.
Discussion
According to the results of the current study, SAB pneumonia foci have a four-fold higher mortality rate than other foci. These findings are consistent with studies that showed high staphylococcal pneumonia mortality rates (9, 10, 11). Mortality from SAB due to a pulmonary focus has been reported to range from 39% to 67%, and the primary focus of infection is known to predict mortality (12). These findings clearly show the need for rapid initiation of appropriate therapy in staphylococcal pneumonia patients. The quick diagnosis of patients is thus another crucial issue. Sometimes a chest X-ray may be insufficient to make a diagnosis. Thoracic CT is not commonly used in patients with staphylococcal bacteremia, and its necessity is controversial. However, a decision should be made in light of the patient’s complaints, symptoms, and physical examination. Based on our results, it is crucial to culture from pulmonary secretions (sputum, endotracheal aspirate).
The central catheter was the most frequent source of infection in this study, as it was in many others. In our study population, chronic renal failure was the most prevalent comorbidity. Hemodialysis patients are well known to have a high risk of SAB (13). The second most common cause of death was SAB focused by a central catheter. Recent studies showed that the access route to dialysis in SAB is crucial. It has been reported that entering hemodialysis via a fistula rather than a central catheter carries less risk (14, 15). In the study population, 80% of hemodialysis patients received hemodialysis through a central catheter. It is well known that the central catheter poses a greater risk than a fistula because of frequent hand contact and that skin colonization is more common in these patients. Therefore, switching to a fistula as soon as possible is advised. Patients on hemodialysis have lower late mortality and higher early mortality rates (16). However, SAB causes invasive infections and high mortality rates than all causes (such as endocarditis and osteomyelitis).
Interestingly, our study’s second most common focus was the intraabdominal source. The high number of patients with intraabdominal malignancy in our facility might have caused this outcome; about half of our patients had abdominal imaging. In addition, patients in the SAB group’s intraabdominal focus typically had prior surgery. Gram-negative bacteria are commonly the causative agent in intraabdominal infections, as is well known. This result could be related with the nosocomial incisional surgical site infections. We noted a low mortality rate in the intraabdominal focus group. Similarly, Laupland et al. reported a low mortality rate in the intraabdominal focus group (17). Even so, clinicians should remember that managing SAB requires early source control.
Recent studies have shown that ID specialist consultation affects survival (3, 18, 19). In our hospital, the clinician should consult an ID specialist to administer antimicrobial therapy when there is a blood culture signal. Our hospital’s rate of ID consultation within the first 96 hours of index blood culture was about 80%; however, this high rate was unaffected by 7-day and 30-day mortality rates. Our study’s unknown focus rate was low because of the high rate of ID consultation. In the study of Kaech et al., the ID consultation rate was 82%, but the unknown focus was 52% (20). In contrast, Kaash et al. reported a high mortality rate in the unknown focus; in addition, they recommended new imaging techniques, such as positron emission tomography/computed tomography (PET/CT), when traditional methods failed to detect focus (21). However, there is currently insufficient evidence to require using PET/CT or other novel imaging techniques.
On the other hand, echocardiography imaging is definitely recommended in patients with SAB, while other imaging methods are recommended based on the patient’s history and physical examination (22, 23). Transthoracic echocardiography should be performed first to identify cardiac involvement. Patients at risk or suspected of having infective endocarditis should have TEE. In our study, the number of patients who were not performed echocardiography was significantly high among the non-survivors.
This study also aimed to evaluate the approach to SAB in our hospital. The rate of our repeat blood culture at any time was above 80%, and the negativity control in 7 days rate was 78%. It is well known that persistent SAB, despite appropriate antibiotic therapy, is prognostically significant. For example, in a large European cohort of over 900 patients, 32% of cases had bacteremia for at least one additional day after beginning appropriate antibiotic therapy, and 30-day mortality was twice that of patients whose blood cultures cleared immediately (28% vs. 13%) (24).
Despite having a high ID consultation rate, a high negativity rate of repeat blood culture, and a high TTE imaging rate, our mortality rates were similar to those reported in the literature. Our appropriate maintenance treatment rate is 72%, which usually depends on the continuation of glycopeptide therapy in critically ill patients despite MSSA. This finding suggested that cefazolin may outperform glycopeptides in treating MSSA, as Wong et al. (25) reported. However, large-scale prospective randomized trials on this topic are required.
Our study has some limitations. First, despite its long duration, it is limited by retrospective design and single-center setting. Second, local factors (such as patient population and local resistance rates) vary between studies. Finally, the fact that we had only the last episode in patients with recurrent bacteremia attacks may have increased our mortality rate.
In conclusion, despite appropriate antibiotics and medical interventions, staphylococcal bactereimia remains a severe infection. Several prognostic factors influence mortality (such as host factors, pathogen-related factors, and host interaction). SAB is still a threat, and its prevalence appears to increase with foreign bodies (such as prostheses and artificial heart valves). Identifying the source, ensuring source control, and appropriate initial therapy as soon as possible are critical for reducing mortality and morbidity in SAB. Up-to-date and standardized guidelines are required for the management of SAB.