Introduction
Coronavirus disease 2019 (COVID-19) is a disease with a wide clinical spectrum ranging from mild to moderate illness to acute respiratory distress syndrome (ARDS) and death. Approximately 25% of patients with COVID-19-related ARDS required mechanical ventilation due to respiratory failure and were treated in intensive care units (ICUs) (1). While the overall mortality rate in the ICU is around 60%, the mortality rate in patients receiving mechanical ventilation is higher, ranging from 24% to 80% (2).
Despite advances in antimicrobial treatment, supportive care, and preventive measures, the mortality rate for patients who develop ventilator-associated pneumonia (VAP) remains around 13%. VAP is a morbidity and mortality factor that affects the clinical course of approximately 10% of patients in the ICU (3). The development of VAP is more frequent in patients with COVID-19-related ARDS (4). Mortality rates are observed to be higher in patients who develop VAP during COVID-19 (5). This study aimed to identify risk factors for mortality on day 14 of hospitalization, risk factors for VAP development, factors affecting mortality in patients who developed VAP, and to assess antimicrobial resistance patterns of isolated pathogens in mechanically ventilated patients with COVID-19.
Materials and Methods
A retrospective observational cohort study was designed to evaluate COVID-19-positive patients developing VAP. Patients aged ≥18 who received COVID-19 treatment in the ICU while receiving ventilator support between July 2020 and July 2021 were analyzed. Patients who tested negative for COVID-19 RT-PCR, were followed outpatient for COVID-19, had bacterial pneumonia upon ICU admission, or had been on mechanical ventilation for less than two days were excluded from the study. Kayseri City Hospital Clinical Research Ethics Committee approved the study on August 22, 2023, with the decision number 889.
Demographic data, risk factors, comorbidities, acute physiology and chronic health evaluation (APACHE) II scores, administered anti-inflammatory agents, antibiotics, and durations were recorded for patients hospitalized with COVID-19 pneumonia. Endotracheal aspirate cultures and sensitivity results were collected along with
VAP was diagnosed in patients who developed at least two of the following symptoms or signs after 48 hours of mechanical ventilation: new-onset fever (≥38°C) or hypothermia (≤36°C), new or increased respiratory secretions, leukocytosis or leukopenia, increased minute ventilation rate, decreased arterial oxygenation, increased requirement for vasopressor infusion to maintain target blood pressure, or new or progressive infiltrates on chest radiographs or computed tomography (CT) scans (6).
Microbiological investigation was performed on endotracheal aspirate (ETA) samples, and any significant growth with a colony-forming unit (CFU) count of ≥105/mL was identified using the VITEK 2 system (bioMérieux, France). Antimicrobial susceptibility testing of the isolated bacteria was tested using the standard disc diffusion method (modified Kirby-Bauer technique) on Muller-Hinton agar, according to guidelines of the European Committee on Antimicrobial Susceptibility Testing (EUCAST). The disk elution method was used to determine colistin susceptibility in carbapenem-resistant isolates.
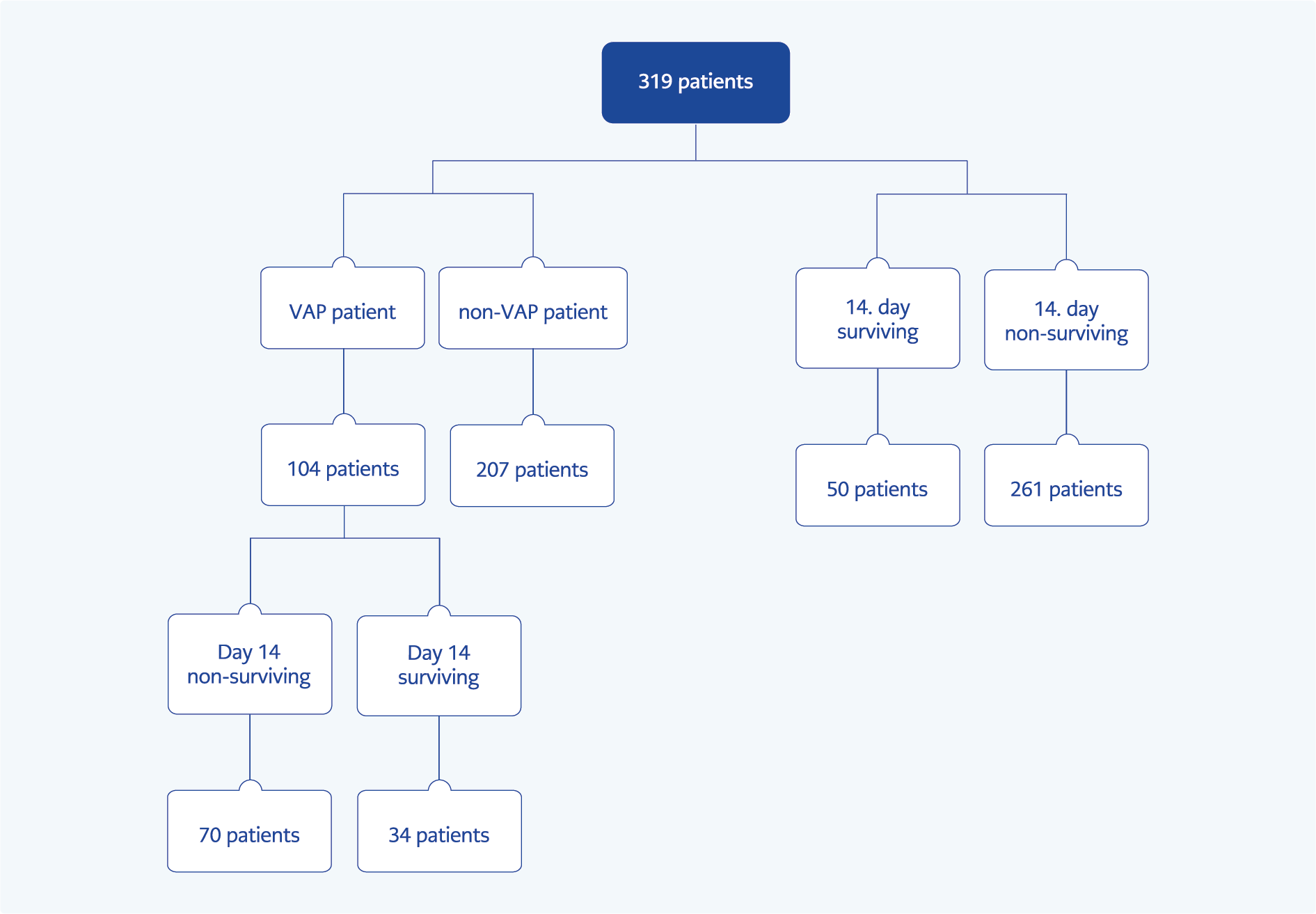
Statistical analysis was performed using IBM SPSS Statistics for Windows, Version 25.0 (IBM Corp., Armonk, NY, USA). Chi-square or Fisher’s exact test was used for comparisons of categorical variables. Normality was assessed using the Shapiro-Wilk test and histogram analysis. Parametric data were analyzed using Student’s t-test for comparisons between groups, while non-parametric data were analyzed using the Mann-Whitney U test. Binary logistic regression was applied to dependent categorical variables. Patients were classified into three groups based on survival on day 14, the development of VAP, and survival on day 14 for patients who developed VAP. The demographic characteristics, immunosuppressive and antibiotic treatments, pathogen resistance patterns, and prognosis of these groups were compared.
Results
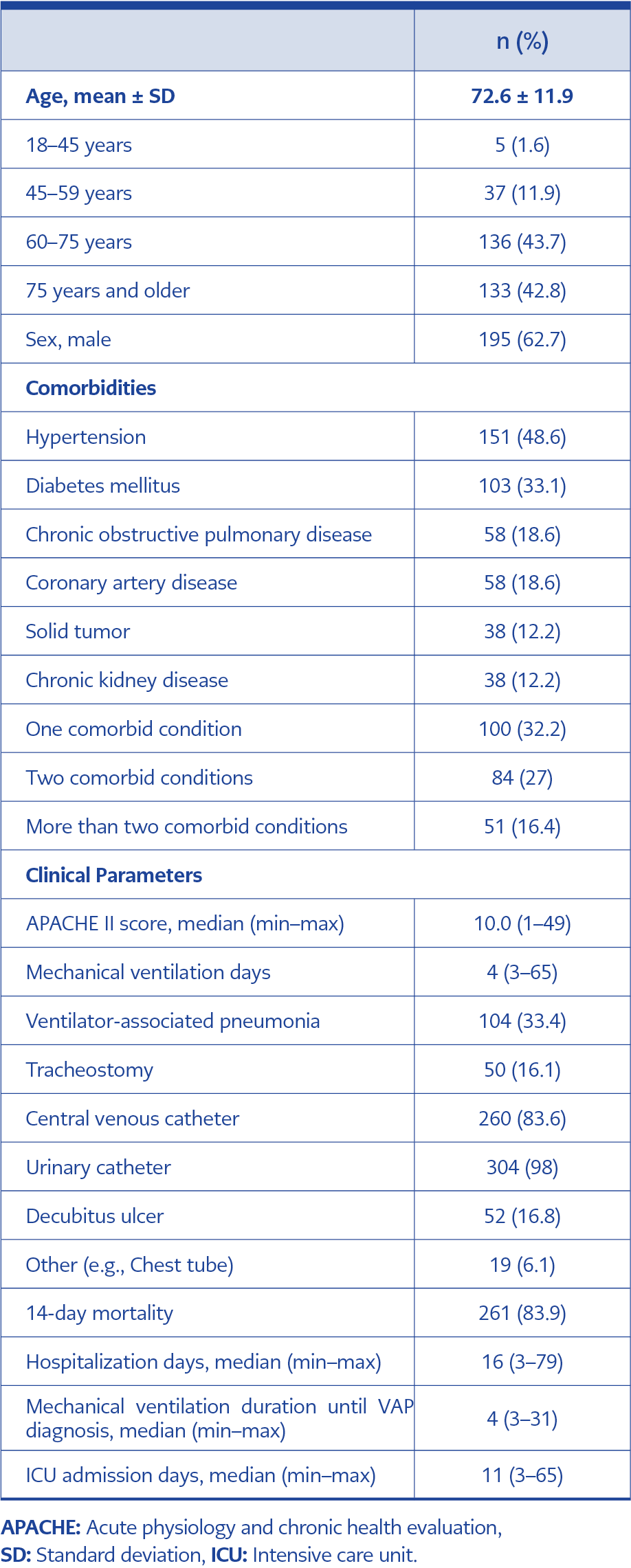
A total of 339 patients were analyzed during the study period. After excluding 28 patients with an ICU stay of less than 48 hours, 311 patients were included in the final analysis (Figure 1). The mean age was 72.6 ± 11.9 years, and 62.7% of the patients were male. The median APACHE II score was 10. A comorbid condition was present in 32.2% of patients, with hypertension being the most frequent comorbidity (48.6%). Of patients, 83.9% had died by day 14. The median hospital stay for the patients was 16 days, while the median ICU stay was 11 days. VAP was detected in 33.4% of the patients.
Regarding COVID-19 treatment, 77.2% of the patients received corticosteroids: 32.5% received dexamethasone only, and 56.6% received methylprednisolone (MP) only. Additionally, 17.7% were treated with tocilizumab, and 15.4% received pulse steroid therapy (>250 mg/day). The demographic and clinical characteristics of the patients are presented in Table 1.
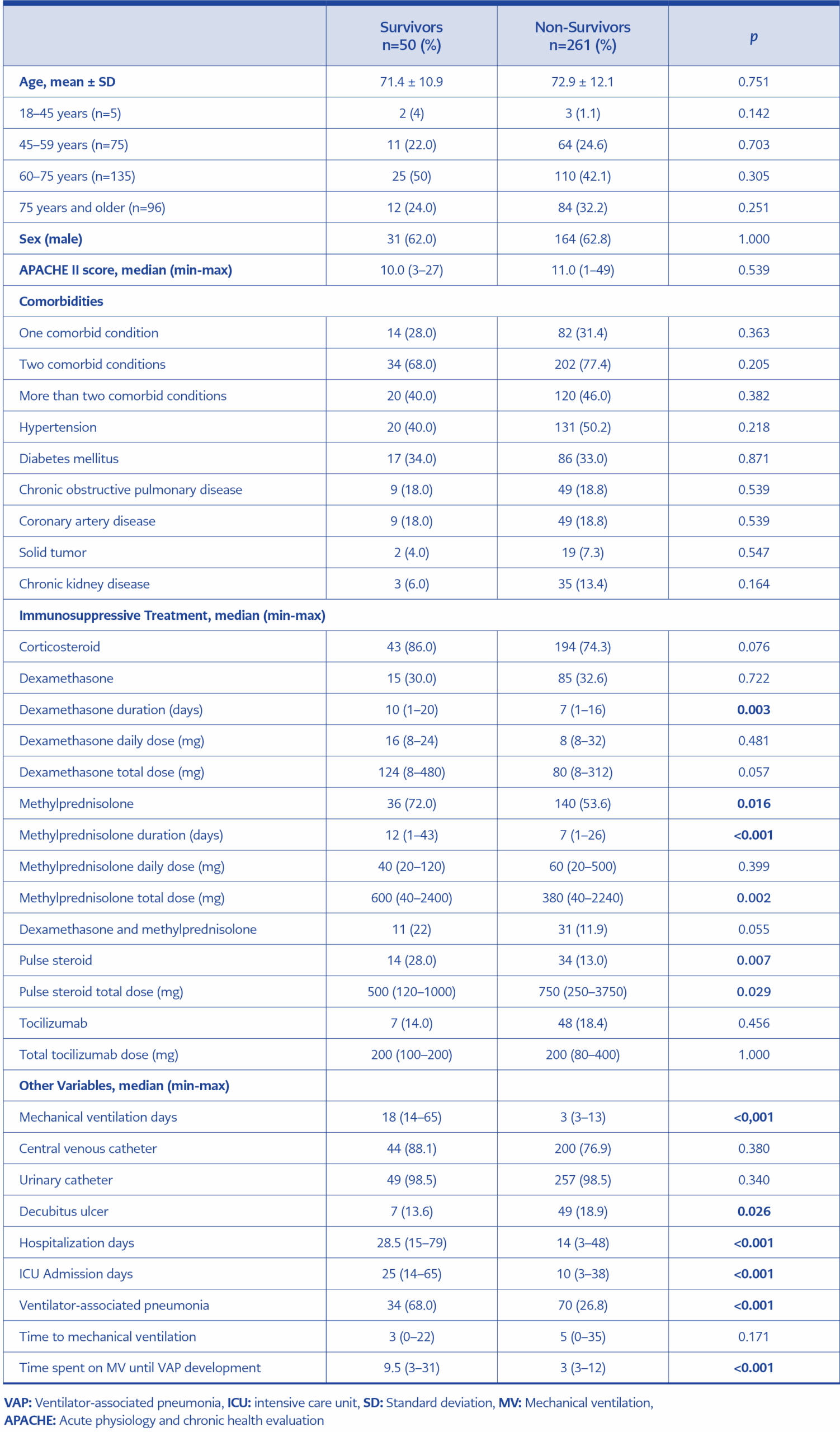
The patients included in the study were evaluated for 14-day mortality and divided into two groups: survivors and non-survivors. The characteristics of the groups are shown in Table 2. Steroids were administered to 74.3% of the non-survivors and 86% of the survivors for the treatment of COVID-19. The duration of dexamethasone use was significantly longer in the non-survivor group (p=0.003). However, MP use was more common among the survivors (p=0.016). The median duration of MP use was significantly longer in the survivor group (p<0.001), with a median total dose of 600 mg, which was significantly higher (p=0.002) compared to the non-survivor group. Furthermore, pulse steroid therapy was administered to 13% of the non-survivors and 28% of the survivors (p=0.007). The total dose of pulse steroids was significantly higher in the non-survivor group. VAP was detected in 68% of the survivors, which was significantly higher than in the non-survivors (p<0.001) (Table 2).
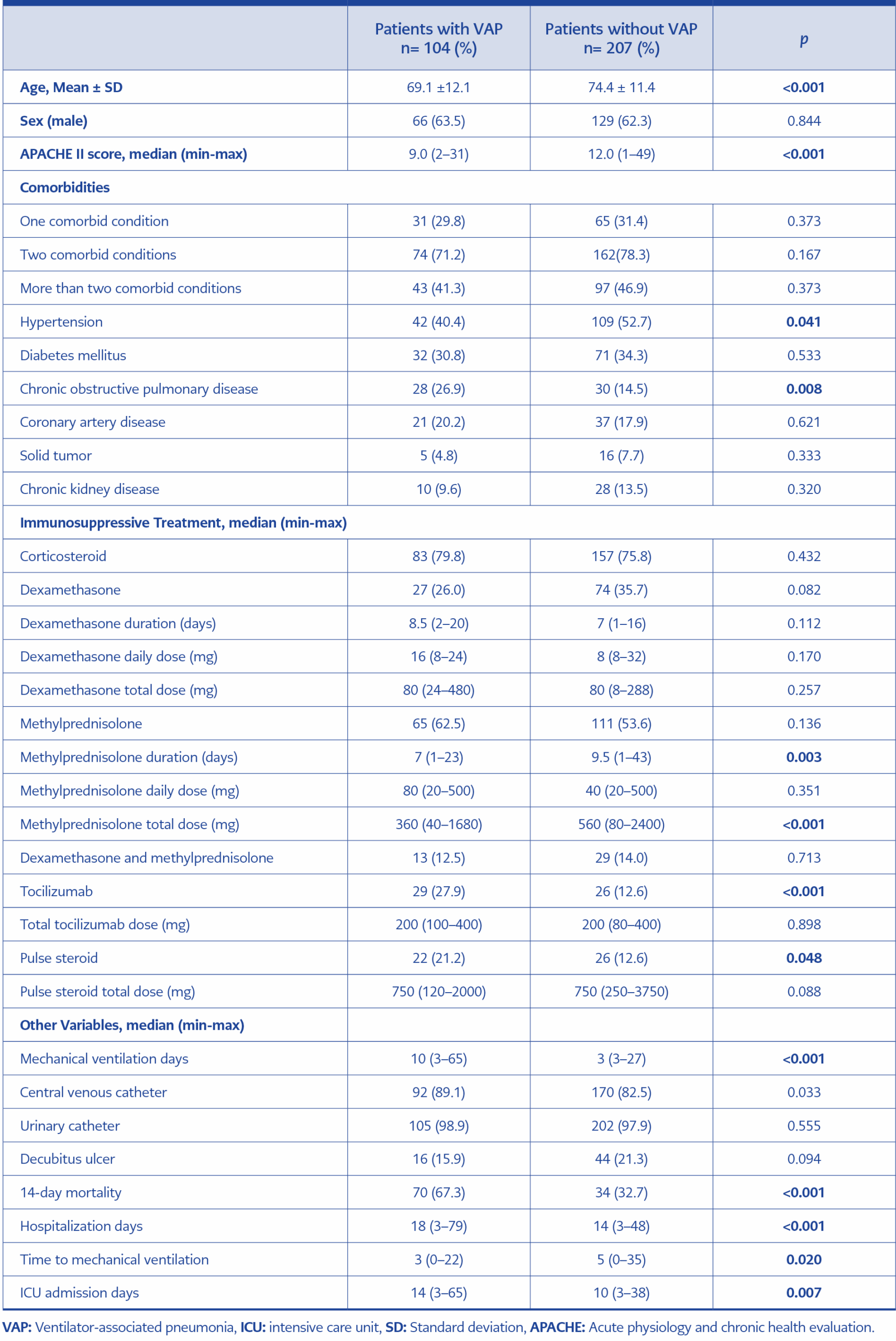
The patients were also divided into two groups based on the development of VAP: VAP and non-VAP groups. It was found that the incidence of VAP was higher in the older age group (p<0.001). The APACHE II score was significantly lower in the VAP group, with a median score of 9 (range, 2–31; p<0.001). Hypertension was present in 52.7% of patients without VAP (p=0.041). Chronic obstructive pulmonary disease (COPD) was observed in 26.9% of patients with VAP, which was significantly higher compared to those observed in 14.5% of the non-VAP group (p=0.008) (Table 3). In the binary logistic regression analysis, the likelihood of developing VAP was 2.4 times higher in those with COPD (95% confidence interval [CI], 1.32–4.34; p=0.004). Among patients who developed VAP, the median duration of MP use was 7 days (p=0.003), and the total dose was significantly higher (p<0.001). A higher proportion of patients who developed VAP (27.9%) received tocilizumab compared to the non-VAP group (p<0.001). Additionally, 21.2% of patients with VAP received pulse steroid therapy, which was significantly higher than in the non-VAP group (p=0.048). A comparison of the patient groups with and without VAP is presented in Table 3.
Among the patients who developed VAP, two subgroups were formed based on 14-day survival: survivors and non-survivors. In the non-survivor group, the median duration of dexamethasone use was 7 days, shorter than that in the survivors, while the daily dose was higher, with a median of 16 mg (p=0.024). Similarly, the median duration of MP use was 7 days in the non-survivor group, significantly shorter than in the survivors (p=0.003).
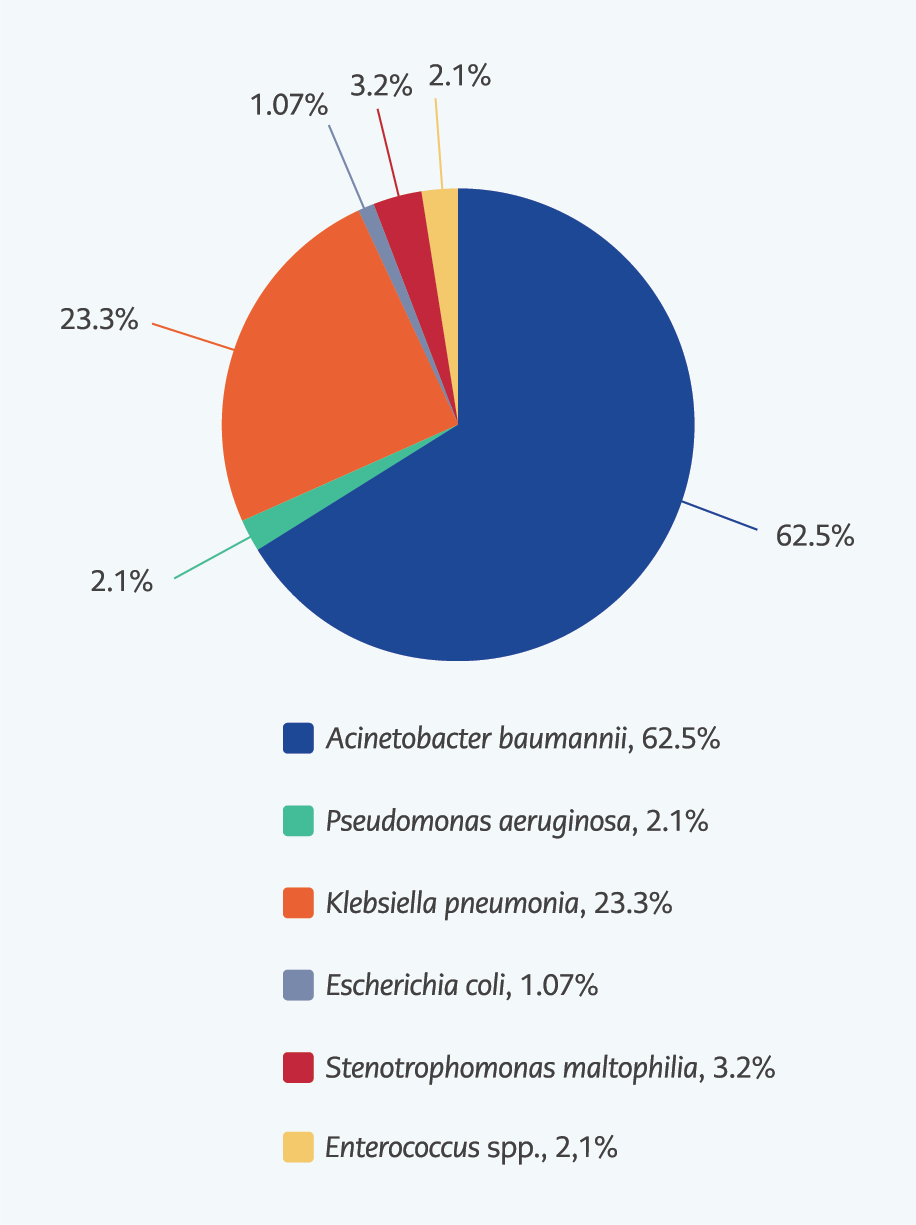
In patients who developed VAP, 56.7% (n=59) had positive endotracheal aspirates (ETA) cultures. Among those with positive ETA cultures, 64.4% were in the non-survivor group. The most frequently isolated microorganism in the non-survivor group was Acinetobacter baumannii, accounting for 28.5% (20/38) of cases, followed by Klebsiella pneumoniae at 11.4% (8/38) (p=0.199 and p=0.635, respectively). Of the isolated bacteria, 96.3% were Gram-negative, while 3.7% were Gram-positive. The most frequently isolated Gram-negative pathogen was A. baumannii at 62.5% (n=35), and the most common Gram-positive pathogen was Enterococcus spp. at 3.7% (n=2) (Figure 2).
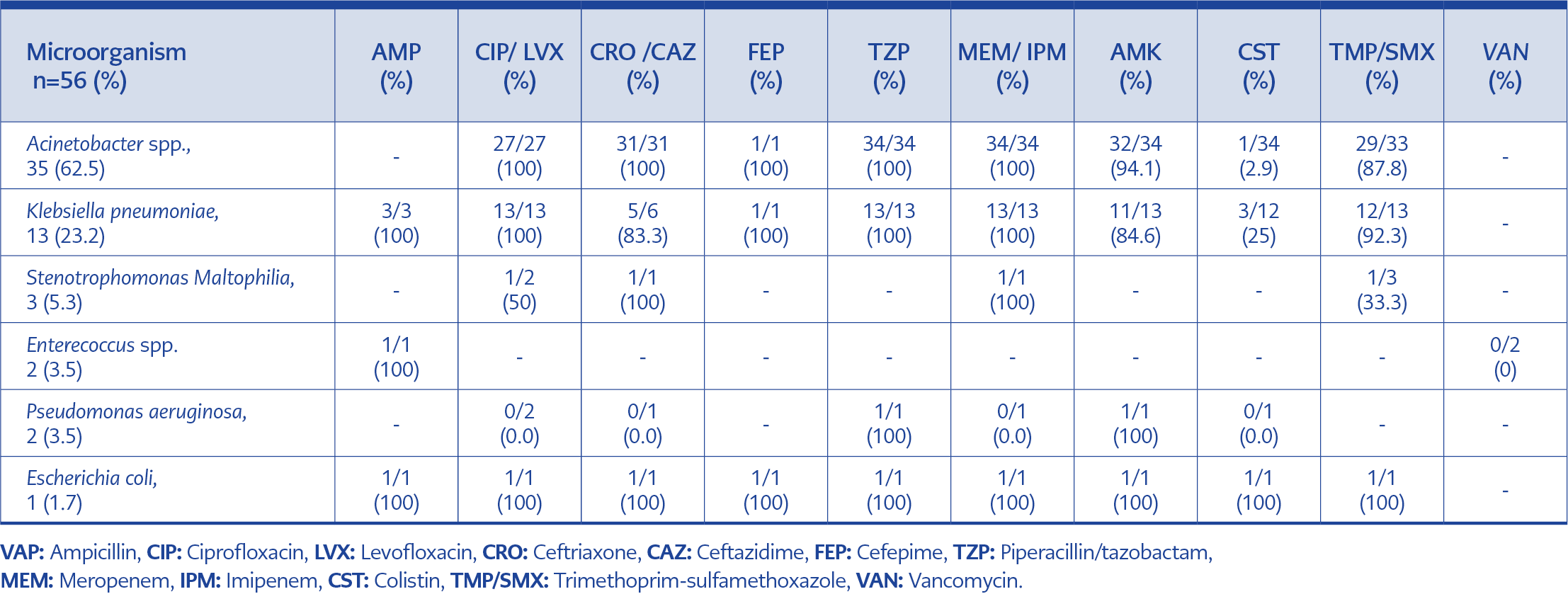
Resistance to fluoroquinolones was observed in 100% of Escherichia coli and K. pneumoniae strains and 50% of Stenotrophomonas maltophilia strains. Resistance to third-generation cephalosporins was found to be in 100% of Acinetobacter spp. strains and in 83.3% of K. pneumoniae strains. All strains of A. baumannii, K. pneumoniae, and E. coli were resistant to carbapenems. Colistin resistance was detected in A. baumannii at a rate of 2.9% and in K. pneumoniae at 25%. No colistin resistance was observed in Pseudomonas aeruginosa or E. coli. Additionally, vancomycin resistance was found in Enterococcus spp. The distribution of isolates and the antimicrobial resistance rates in VAP patients are shown in Table 4.
On day 14, the antibiotic regimens administered to the patients with VAP included macrolides in 59.6% (62/104), cephalosporins in 36.5% (38/104), beta-lactam/beta-lactamase inhibitors in 33.7% (35/104), quinolones in 17.3% (18/104), carbapenems in 15.4% (16/104), glycopeptides in 10.6% (11/104), colistin in 1.9% (2/104), and other antibiotics in 1% (1/104). The most commonly used class of antibiotics in the VAP patient group was macrolides. There was no statistically significant difference in empirical antibiotic preferences between the survivor and non-survivor patient groups (p>0.05). Empirical antibiotic changes were made in 91.4% of the non-survivor group; however, no statistically significant difference was found between the survivors and non-survivors (p=0.282). The 14-day mortality rate was 1.17 times higher in patients without a treatment change compared to those with a treatment change (95% CI, 1.08–1.27; p=0.015).
Discussion
COVID-19 has caused significant health issues globally, leading to mortality and morbidity in millions of individuals. This study primarily included patients with severe illness and an advanced average age. Among the survivors, the use of MP was more common, and the median duration and total dose of MP were significantly higher compared to the non-survivor group. COPD was observed in patients with VAP, and this was significantly higher compared to those without VAP. The risk of developing VAP was 2.4 times higher in patients with COPD. Furthermore, in patients who developed VAP, the median duration of MP use and the total dose were significantly higher. A higher proportion of patients who developed VAP received tocilizumab (27.9%) and underwent pulse steroid therapy (21.2%), both of which were significantly more common compared to the non-VAP group. The most frequently isolated Gram-negative pathogen was A. baumannii (62.5%).
Older adults, particularly those with comorbidities, have been more severely affected by COVID-19. Hypertension in COVID-19 patients has been associated with increased need for ICU admission, invasive ventilation, and higher mortality (7). In the Philippine CORONA study, among 10,881 patients, 3647 (33.5%) had hypertension (8). In our study, similar to the literature, hypertension was the most frequently observed comorbidity in all patient groups.Treatment in COVID-19 patients aims to prevent the excessive and disproportionate hyperinflammatory response initiated by the host (4). In the early stages of the pandemic, the randomized controlled RECOVERY trial administered 6 mg/day of dexamethasone for 10 days to 2104 COVID-19 patients, while 4321 patients were followed as a control group. The trial observed a reduction in 28-day mortality and duration of hospital stay, particularly in patients who required mechanical ventilation. No association was found between steroid use and mortality in patients not receiving oxygen therapy, and therefore, steroid treatment was not recommended for this group (9).
A retrospective controlled study in Türkiye involving 450 COVID-19 patients divided them into three groups: standard care, high-dose steroid therapy (6 mg/day equivalent of dexamethasone), and pulse steroid therapy (250 mg/day MP). The average ICU stay was 9.0 (95% CI, 6.0–12.0) days in the standard care group, 8.0 (95% CI, 5.0–13.0) days in the high-dose steroid group, and 4.5 (95% CI, 3.0–8.0) days in the pulse steroid group (10). In another study, after corticosteroid initiation, the ICU admission rate (4.8% vs. 14.4%) and mortality (9.5% vs. 17.1%) were lower in the MP group (11). This study observed higher usage of MP and dexamethasone in all surviving patient groups. Furthermore, in the VAP patient group, the duration and total dose of MP use were higher.
A meta-analysis evaluating seven studies found that tocilizumab therapy did not reduce mortality in severe COVID-19 cases (12). However, De Rossi et al. (13) demonstrated that early and low-dose tocilizumab therapy reduced mortality compared to standard treatment in patients with COVID-19-related respiratory failure. IL-6 antagonists cause a temporary but prolonged immunosuppressive state, which can facilitate the development of bacterial superinfections like VAP (14). In this study, the use of pulse steroids and tocilizumab was higher in the VAP group, suggesting that immunosuppressive therapy may have contributed to the development of VAP. Additionally, in terms of 14-day mortality, consistent with the literature, the rate of pulse steroid use was higher in the survivor group.
Ippolito et al. (15) conducted a meta-analysis on the frequency of VAP in COVID-19 pneumonia, estimating the VAP rate to be 45.4% (95% CI, 37.8–53.2; 2611/5593 patients; I²=96%) in these patients. Additionally, mortality in critically ill COVID-19 patients has been reported to range between 30% and 60% in the literature (16). In our study, a lower rate of VAP (33.4%) was observed compared to the literature. Despite the lower VAP rate, the mortality rate was found to be extremely high (98%). The high mortality rate may be attributed to the high proportion of elderly patients, comorbidities, and the immunosuppressive treatments administered. Notably, 86.9% of the patients followed in the ICU were over 60 years old, which may have contributed to the high mortality rate.
In ICUs, 80% of carbapenem-resistant A. baumannii (CRAB) isolates are recovered from sputum specimens, with CRAB accounting for more than 50% of the carbapenem-resistant Gram-negative bacilli. The genetic transfer of resistance in Gram-negative bacteria plays a crucial role in the dissemination of antibiotic resistance and occurs through various mechanisms, including conjugation, transformation, and transduction (17). In a separate study, A. baumannii was the predominant bacterium, representing 43.8%, and all identified pathogens were multidrug-resistant (MDR) (18). In our study, the most prevalent pathogen in VAP was CRAB, and other pathogens were MDR, likely contributing to the high fatality rate. Another contributing factor may have been the overwhelming capacity of hospitals and ICUs during the peak of the pandemic, which resulted in critically ill patients being monitored in general wards and transferred to the ICU in the later stages of illness.
In a study of 352 critically ill COVID-19 patients, the duration of mechanical ventilation was 16 days (interquartile range [IQR], 8–28), the duration of ICU stay was 18 days (IQR, 9–29), and the 28-day mortality was 32.1% (19). In our study, however, the total hospital and ICU stays were shorter in the non-survivor patient group on day 14 compared to the survivor group, suggesting that the non-survivors had more critical disease, which contributed to the higher mortality rate. On day 14 of post-mechanical ventilation, the average APACHE II score of the non-survivors was higher than that of the survivors.
The average duration of mechanical ventilation and the time spent on mechanical ventilation until VAP onset were shorter in the non-survivor group compared to the survivors. Similarly, the VAP patients in the non-survivor group had shorter ICU stays and mechanical ventilation durations on day 14. Consistent with the literature, the total duration of hospital stay was longer in the VAP group. These patients had risk factors such as prolonged ICU stays and extended mechanical ventilation, which contributed to the development of VAP. When 14-day mortality after mechanical ventilation was calculated, 67.3% of the non-survivors had developed VAP. This finding supports that VAP is a significant factor that increases mortality. On day 14 of hospitalization, VAP was detected in 68% of surviving patients (34/50), which was higher than in the non-survivor group. The lower VAP rate in the non-survivor group suggests that the high mortality rate was the primary factor. Due to the short duration of stay in the ICU, patients often were exitus before developing VAP.
In a study examining bacterial co-infections in COVID-19 patients, fluoroquinolones and cephalosporins were found to constitute 74% of the antibiotics used (20). Similar to the literature, in our study, the most commonly used antibiotics were macrolides, cephalosporins, beta-lactam/beta-lactamase inhibitors, quinolones, carbapenems, glycopeptides, and colistin. There was no statistically significant difference between the antibiotic regimens when comparing the 14-day mortality and survival rates of the groups. However, a significant difference was observed in the treatment change. In this study, mortality was 1.17 times higher in patients whose treatment regimen was not changed.
In a different study assessing VAP pathogens, Gram-negative bacilli were identified as the most frequently isolated pathogens, with Enterobacter spp. and P. aeruginosa being the most prevalent (4). Karataş et al. (21) showed that A. baumannii was the dominant pathogen in lower respiratory tract cultures during the pandemic, and the percentage of E. coli isolates decreased. However, the Gram-negative bacterial profile in COVID-19 patients can vary regionally. For instance, a study conducted in Brazil identified K. pneumoniae as the predominant Gram-negative bacterium in cultures (22). The incidence of A. baumannii was reported as 4.4% by Nseir et al. (23), 7.3% by Rouzé et al. (24), and 27.4% by Meawed et al. (25). In a recent study comparing the distribution of pathogens from tracheal aspirate cultures during the pandemic to the pre-pandemic period, an increase in A. baumannii was observed, while K pneumoniae and P. aeruginosa showed a decrease (26). In line with the literature, we found that 96.3% of the isolated bacteria were Gram-negative, with Gram-positive bacteria constituting only 3.7%.
However, in contrast to the literature, the most frequently isolated Gram-negative pathogen was A. baumannii, at 62.5%. This may be due to the failure of infection control measures and routine procedures during the COVID-19 pandemic, which facilitated the spread of resistant strains. For example, confusion over hand hygiene protocols and double-glove use among healthcare workers may have contributed. Additionally, the increased patient load in ICUs might have led to inadequate environmental sterilization, promoting colonization. Known risk factors for A. baumannii infections, such as mechanical ventilation, prolonged antibiotic use, and steroid therapy, were frequently applied in critically ill COVID-19 patients (27). In our center, the carbapenem resistance rate has been 97.9% for K. pneumoniae and 99.7% for A. baumannii. Additionally, the hand hygiene compliance rate in 2020 was 81.7%, and in 2021, it was 82.9%, contributing to the spread of resistant pathogens.
Sharifipour et al. (28) reported that A. baumannii isolates from COVID-19 patients showed high resistance to all antibiotics except colistin, with 52% resistance. In this study, A. baumannii showed 2.9% resistance to colistin, with 100% resistance to third-generation cephalosporins and carbapenems. Li et al. (29) reported a 76.6% resistance rate of K. pneumoniae to carbapenems in COVID-19 patients. A study conducted in Italy found that carbapenem-resistant strains of K. pneumoniae were 6.7% in 2019, while during the pandemic in 2020, the resistance rate increased to 50% (30). In this study, the resistance of K. pneumoniae to third-generation cephalosporins and carbapenems was found to be high, while colistin resistance was lower. The most important risk factors for carbapenem-resistant K. pneumoniae infections are mechanical ventilation and central venous catheter use, which are frequently applied in COVID-19 patients, explaining the prevalence of resistant strains isolated from respiratory and blood cultures.
The use of MP and pulse steroids by day 14 was effective in survival. In COPD patients, the incidence of VAP was higher, highlighting the careful monitoring following intubation. Additionally, patients receiving long-term and high-dose MP, as well as those receiving tocilizumab and pulse steroids, should be closely monitored for the development of VAP. All strains of A. baumannii were resistant to carbapenems, while colistin resistance was detected at 2.9%. Based on these findings, infectious disease specialists should consider resistance rates when selecting treatment and managing patients. Immunosuppressive therapy by day 14 reduces mortality but increases the risk of VAP and mortality due to MDR pathogens. Therefore, early detection of infections, timely weaning from the ventilator, and appropriate discharge from the intensive care unit will reduce the mortality risk in these patients.
The main limitation of the study is its retrospective, single-center design, which limits generalizability. The small sample size, particularly in subgroup analyses, restricted detailed analysis and comparison. Additionally, the high ICU occupancy during the pandemic period caused many patients to be monitored in the general wards until the need for intubation arose.
Patients receiving immunosuppressive therapy should be closely monitored for the development of VAP. In patients with VAP, empirical treatment should be planned considering the possibility of resistant Acinetobacter spp. infections. Early detection of infections, timely weaning from the ventilator, and appropriate discharge from the intensive care unit will reduce the mortality risk in these patients. The mortality rate was higher in patients with VAP who received tocilizumab. This may be associated with a higher tendency to initiate tocilizumab therapy in patients with a more severe clinical course. Although pulse steroid use was more common among patients with VAP, those who received pulse steroids had significantly lower mortality rates compared to those who did not. Antibiotic selection in ICUs should be based on the increasing incidence of A. baumannii and carbapenem resistance among pathogens observed in these units.