Introduction
Elevated procalcitonin levels are associated with increased bacterial infection rates in children and adults (1, 2). Identification of bacterial infection in previous studies has used procalcitonin thresholds of 0.5 ng/mL-1.0 ng/mL (2, 3). Procalcitonin level elevations have been reported in COVID-19 patients; rates of superimposed bacterial infections in COVID-19 are reportedly low (4-8).
Herein, we investigate the utility of procalcitonin in the identification of superimposed bacterial infection in pediatric Acute COVID-19 and multisystem inflammatory syndrome in children (MIS-C). We postulate that when compared to children without COVID-19-related illnesses, children with acute COVID-19 or MIS-C would have a lower positive predictive value of an elevated procalcitonin level. The positive predictive value of procalcitonin in identifying bacterial infection was our primary outcome.
Materials and Methods
We collected data on consecutive patients under 21 years (n=215) admitted to our tertiary children’s hospital between February 1, 2013, and July 15, 2020, who had procalcitonin levels measured within 48 hours of admission for this retrospective cohort study. We reviewed data from this timeframe because there was not sufficient electronic data captured for our study before 2013. The study was approved by the Northwell Health Institutional Review Board on October 4, 2020, with the number 20-0318-CCMC, and a waiver of informed consent was granted. Procedures in accordance with the ethical standards of the responsible committee on human experimentation were followed.
The electronic medical record was used to identify eligible patients. Eligible patients underwent chart review to determine clinical data, including age, sex, length of stay, pediatric intensive care unit (PICU) length of stay, duration of antibiotics, use of vasoactive medications, and laboratory values. Laboratory values collected were limited to those obtained within 48 hours of admission. Patients admitted to the neonatal intensive care unit or for elective surgery were excluded. The electronic medical record was used to collect clinical variables, which were managed using REDCap 10.3.7 electronic data capture tools hosted at Northwell Health and analyzed using SAS University Edition 3.8 (SAS Institute, Cary, NC) (9, 10).
Elevation of procalcitonin was defined as >1.0 ng/mL, based on prior literature linking this threshold to confirmed bacterial infections (2, 3). Confirmed bacterial infection was defined as positive blood or urine culture, positive endotracheal culture with significant leukocytosis on Gram stain, soft tissue or bone infection, or pneumonia diagnosed by chest radiograph in patients. A patient was considered uninfected if there was a positive blood culture but no antibiotic treatment, as a clinician judged the blood culture to represent a contaminant. Suspected bacterial infection was defined as confirmed bacterial infection or administration of therapeutic antibiotics for >48 hours. The 48-hour duration was used to exclude children who received antibiotics purely pending the final result of a negative blood culture, which in our institution results at 48 hours.
Results
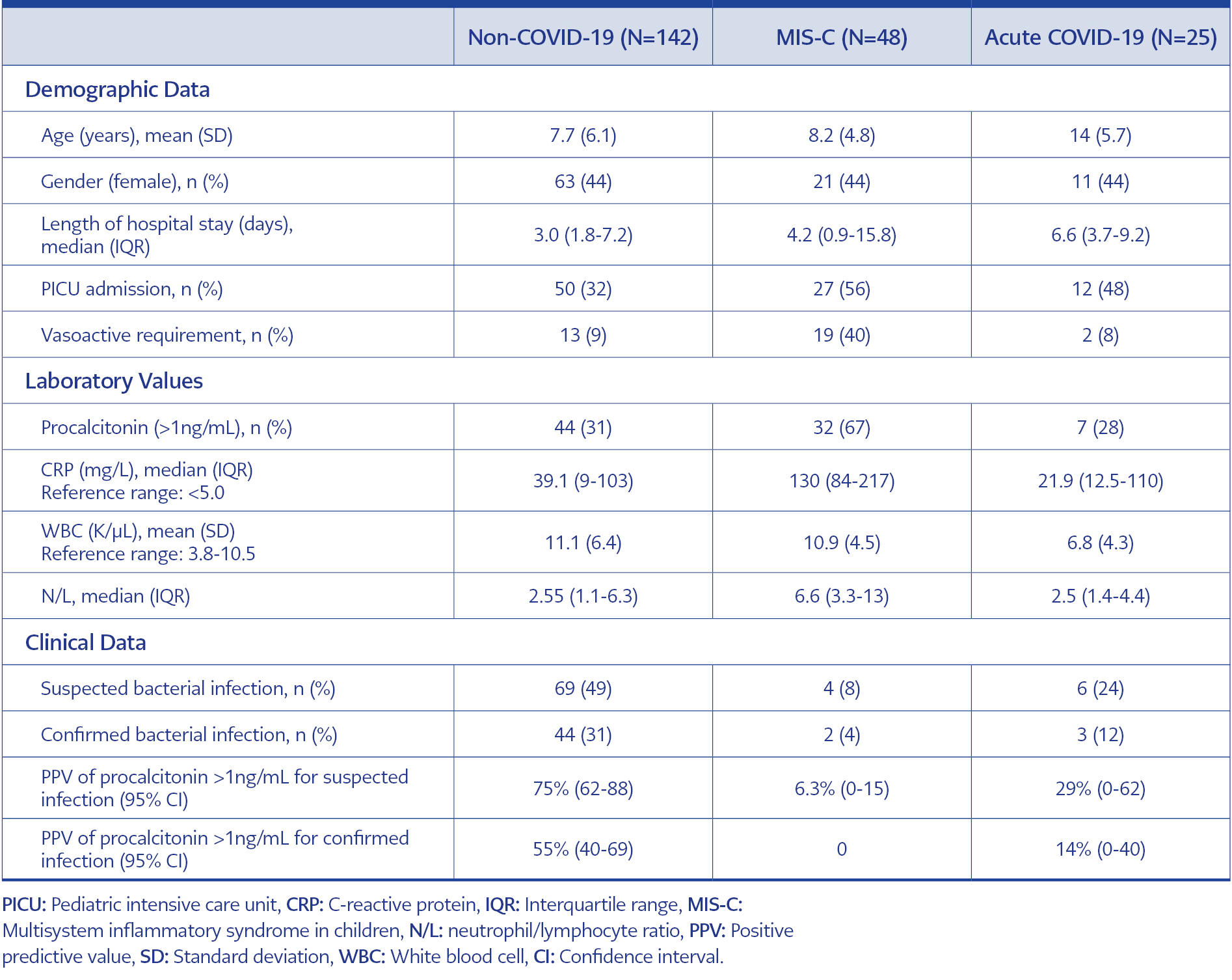
Of 215 patients, 142 (66%) had non-COVID-19-related illnesses, 48 (22%) were diagnosed with MIS-C, and 25 (12%) were diagnosed with acute COVID-19 infection. Of those with MIS-C, 56% required PICU admission, and 40% received vasoactive medications. Of those with acute COVID-19 infection, 48% required PICU admission, and 8% required vasoactive medications. Of the non-COVID-19 cohort, 32% were admitted to the PICU, and 9% required vasoactive medications.
Suspected bacterial infections were present in 8% (n=4) of the MIS-C cohort, 24% (n=6) of the acute COVID-19 cohort, and 49% (n=69) of the non-COVID-19 cohort. The cohorts had varying levels of confirmed bacterial infections, which were present in 4% (n=2) of the MIS-C cohort, 12% (n=3) of the acute COVID-19 cohort, and 31% (n=44) of the non-COVID-19 cohort. Bacterial infections noted in those with MIS-C or acute COVID-19 included pneumonia (n=2), soft tissue infection (n=2), and urinary tract infection (n=1).
On analysis of procalcitonin levels >1.0 ng/mL, 67% (n=32) of those with MIS-C, 38% (n=7) of those with acute COVID-19, and 44 (31%) of the non-COVID-19 subjects had increased procalcitonin levels. Beyond procalcitonin, other inflammatory markers are reported across cohorts in Table 1.
The positive predictive value of an elevated procalcitonin level >1.0 ng/mL in identifying a bacterial infection was our primary outcome. In analyzing our primary outcome, we divided patients into those with suspected and confirmed bacterial infections. In suspected bacterial infections, the PPV of an elevated procalcitonin level was 6.3% (95% CI=0-15%) in MIS-C, 29% (95% CI=0-62%) in acute COVID-19, and 75% (95% CI=62-88%) in the non-COVID-19 cohort.
For identification of confirmed bacterial infection, PPV of an elevated procalcitonin level was 0% in MIS-C, 14% (95% CI=0-40%) in acute COVID-19, and 55% (95% CI=40-69%) in the non-COVID-19 cohort.
Discussion
In our retrospective analysis of children hospitalized with MIS-C or acute COVID-19, using a procalcitonin level above 1.0 ng/mL to identify a confirmed or suspected bacterial infection demonstrated a low PPV. The PPV of a procalcitonin level above 1.0 ng/mL in identifying a confirmed or suspected bacterial infection had some utility in children without COVID-19. Nearly one-third of the COVID-19 cohort required vasoactive support, suggesting a high pre-test probability of bacterial sepsis. Previous literature reports higher levels of procalcitonin in children with COVID-19 than levels reported in adults (8, 11). One study utilized a procalcitonin <0.25 ng/mL to guide discontinuation of antibiotics in adults with COVID-19 (12). Our results suggest that procalcitonin levels may have limited utility in predicting bacterial infection in pediatric patients with COVID-19.
This study has some limitations. One limitation includes the inability to make statistical comparisons of the PPV between cohorts; this is because the true gold standard of an elevated procalcitonin in identifying bacterial infection is unknown, making a statistical comparison of calculated PPVs not possible. Second, this is a retrospective study, so we could not control practitioner practice, which likely altered the pre-test probability of bacterial infection and the reported predictive values. Third, our study relied on a review of laboratory values collected during a hospital stay, so we compared procalcitonin levels collected within 48 hours of admission instead of at a standardized time point. Finally, the modest sample size presented limits the ability to draw full conclusions but does suggest further research could be beneficial to the bedside clinician. Even with altered pre-test probabilities, the PPV of procalcitonin in COVID-19 and non-COVID-19 are distinctive, especially considering that more patients in the COVID-19 cohort required vasoactive support. The results of this preliminary study suggest further prospective research is warranted.
In conclusion, we report that procalcitonin levels are elevated in hospitalized children with COVID-19, independent of the presence of bacterial infection. Without other indicators of bacterial sepsis, perhaps procalcitonin alone should not be used to guide antibiotic therapy beyond the 48-hour period if bacterial cultures remain negative. To our knowledge, this is the first study that examines the utility of procalcitonin in identifying bacterial infection in children with COVID-19-associated illnesses. Given the importance of antibiotic stewardship, alternative indicators of bacterial coinfection are required for pediatric acute COVID-19 and MIS-C.