Introduction
Urinary tract infection (UTI) affects approximately 150 million people worldwide every year and is encountered in all age groups (1). Escherichia coli, Klebsiella spp., group B streptococcus, and Enterococcus spp. are the most frequent species. The increase in antibiotic resistance rates among these agents leads to failures in empirical treatment and causes an increase in mortality, morbidity rates, and costs (2). Knowing the antibiotic susceptibility rates of these agents in the community is vital in selecting empirical treatment. Moreover, extended-spectrum β-lactamases (ESBL), especially observed in Enterobacterales species, have become a critical clinical problem in healthcare-associated infections and recently in community-acquired infections (2). Today, antibiotics such as carbapenems are preferred to treat infections caused by ESBL-producing microorganisms. Risk factors of UTIs due to antibiotic-resistant microorganisms include age older than 60 years, prior UTI history, complicated UTI, presence of a urinary catheter, chronic medical conditions, recent hospitalizations or antibiotic treatment (3).
This study aimed to determine the distribution of agents in community-acquired UTIs (CA-UTI), their antibiotic susceptibility, and the risk factors that cause ESBL production in Enterobacterales species. The awareness of the risk factors may increase the success rates in the empirical treatment of CA-UTIs and contribute to the rational use of antibiotics. Knowing the antibiotic resistance rates of the agents will guide the selection of empirical treatment.
Material and Methods
In this study, patients older than 18 years of age who were hospitalized in the Yıldırım Beyazıt University City Hospital Infectious Diseases and Clinical Microbiology Clinic or followed up in the outpatient clinic between February 1, 2019, and February 1, 2020, and diagnosed with CA-UTI and empiric treatment was initiated, were prospectively monitored.
Patients with other concomitant infections, such as pneumonia, catheter-related bloodstream infection, and those diagnosed with asymptomatic bacteriuria were omitted. Patients with polymicrobial growth or who did not exhibit any growth in their urine culture and were assessed to likely have contamination, indicated by a number of growing microorganisms equal to or less than 103 CFU/ml, were excluded. Patients with a history of hospitalization in the last six months, with a urinary catheter or a nephrostomy catheter, with kidney transplantation and patients in the first year of the transplantation, patients in active chemotherapy program for any malignancy, and frequent hospital admissions for malignancy and chemotherapy follow-up were also excluded, too, because they were evaluated as healthcare-associated urinary tract infections (HA-UTI). Patients from nursing homes requiring medical follow-up were not included, but those provided only eating, drinking, and sheltering facilities were included in the study.
Demographic characteristics (age, gender, patient number, date of diagnosis), symptoms (dysuria, pollakiuria, urgency, hematuria, clouding of urine color, urinary incontinence, abdominal pain, nausea, vomiting, fever, shaking chills, changes in consciousness) of the patients were recorded. Comorbidities such as diabetes mellitus, chronic kidney disease, kidney transplantation, immunosuppression, malignancy, neurological diseases, hypertension, and other complicating factors such as pregnancy, benign prostatic hypertrophy, urolithiasis, urological intervention history, neurogenic bladder, anatomical disorder were noted. The history of frequent urinary tract infections, antibiotic use, and staying in a nursing home was inquired.
The empiric antimicrobial initiated for the patients, the suitability of the antimicrobial choice according to the urine and blood culture results, and the duration of antimicrobial therapy were also recorded. Urine and blood cultures were obtained from the patients included in the pyelonephritis group. Agents grown in cultures and their ESBL production were recorded.
Patients admitted to the intensive care unit or who died during their follow-up because of reasons other than urinary infections were excluded from the study.
Definitions and Classifications
Patients with urinary system symptoms such as frequent urination, dysuria, pollakiuria, and urinary incontinence without systemic signs of infection such as fever, chills, nausea, vomiting, and flank pain were considered cystitis. Patients with at least one sign of systemic infection and urinary system symptoms were defined as pyelonephritis. UTI that developed in patients without obstruction, urolithiasis, anatomical disorder, urological pathologies such as a urinary stent, comorbidities such as chronic kidney failure, diabetes mellitus, malignancy, and complicating factors such as immunosuppression was defined as uncomplicated UTI. UTI that developed in patients with any of these factors was considered a complicated UTI (4 ).
The history of two or more UTIs within six months or three or more UTIs within a year was examined for frequent urinary tract infections (5). In diagnosing chronic kidney disease, a glomerular filtration rate of <60 ml/min/1.73 m2 or the need for hemodialysis were used as criteria. Antibiotic usage criteria included using antibiotics for at least 48 hours within the past six months. The use of a maintenance immunosuppression protocol due to malignancy or after solid organ transplantation, use of immunomodulatory drugs for rheumatological, neurological, dermatological diseases, inflammatory bowel diseases, use of any dose of glucocorticoids for more than four weeks were determined as a criterion for immunosuppression.
Sequential Organ Failure Evaluation Score (qSOFA), a bedside clinical evaluation score, was used when sepsis was suspected in patients at the first admission or during follow-up. Sepsis was determined if the patients had two or more criteria of ≥22/min respiratory rate, change in mental status, and systolic blood pressure of ≤100 mmHg (6).
The treatment initiated before the urine culture results was defined as empirical treatment. As a result of the antibiotic sensitivity of the microorganism grown in the urine culture, it was considered ‘empirical treatment suitable’ if it was sensitive to the empirical antibiotic treatment started and ‘empirical treatment not suitable’ if it was resistant.
Microbiological Examinations
Urine and blood culture-antibiograms were studied using traditional methods in the general microbiology laboratory. Identification and antibiotic susceptibility of bacteria were determined using the VITEK-2 Compact (BioMérieux, France) system. According to the antibiotic susceptibility results, resistant and intermediate results were accepted as “resistant,” and sensitive results were considered “susceptible.” ESBL production in E. coli, Klebsiella spp., and Proteus spp. was detected using the double-disc synergy test and evaluated according to Clinical and Laboratory Standards Institute standards. ESBL production was confirmed by using double disc synergy and E-tests (AB Biodisk, Sweden). The double disc synergy test was performed using amoxicillin-clavulanic acid in the center and CAZ, CRO, cefoxitin, and aztreonam around it at a 25 mm distance. Expansion of indicator cephalosporin inhibition zone towards amoxicillin-clavulanic acid disc by double disc synergy method was interpreted as production of ESBL enzyme.
In the study, patients’ demographic characteristics, agents’ distribution, antibiotic susceptibility rates, and the suitability of empirical treatments were examined. Demographic characteristics were statistically investigated between patient groups with CA-UTI attacks by ESBL-producing and non-ESBL-producing species and risk factors for ESBL production were determined.
Statistical Analysis
The statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) 20.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics for categorical variables were presented as numbers and percentages, and for numerical variables, as mean ± standard deviation, minimum-maximum, or median (1st quartile-3rd quartile) values according to the characteristics of the data. The normal distribution of numerical data was examined using the Kolmogorov-Smirnov and Shapiro-Wilk tests. The mean difference between the two independent groups showing normal distribution was analyzed using the independent samples T-test. The Mann-Whitney U test analyzed the median difference between two independent groups that did not show normal distribution. The analyses of categorical variables among themselves were performed with the Chi-square test when the Chi-square condition was met and with Fisher’s exact test if it was not. Univariate, binary logistic and multinominal logistic regression tests were used in model selection. The tests were considered statistically significant if the p-value was less than 0.05 by examining the data at the 95% confidence level.
Results
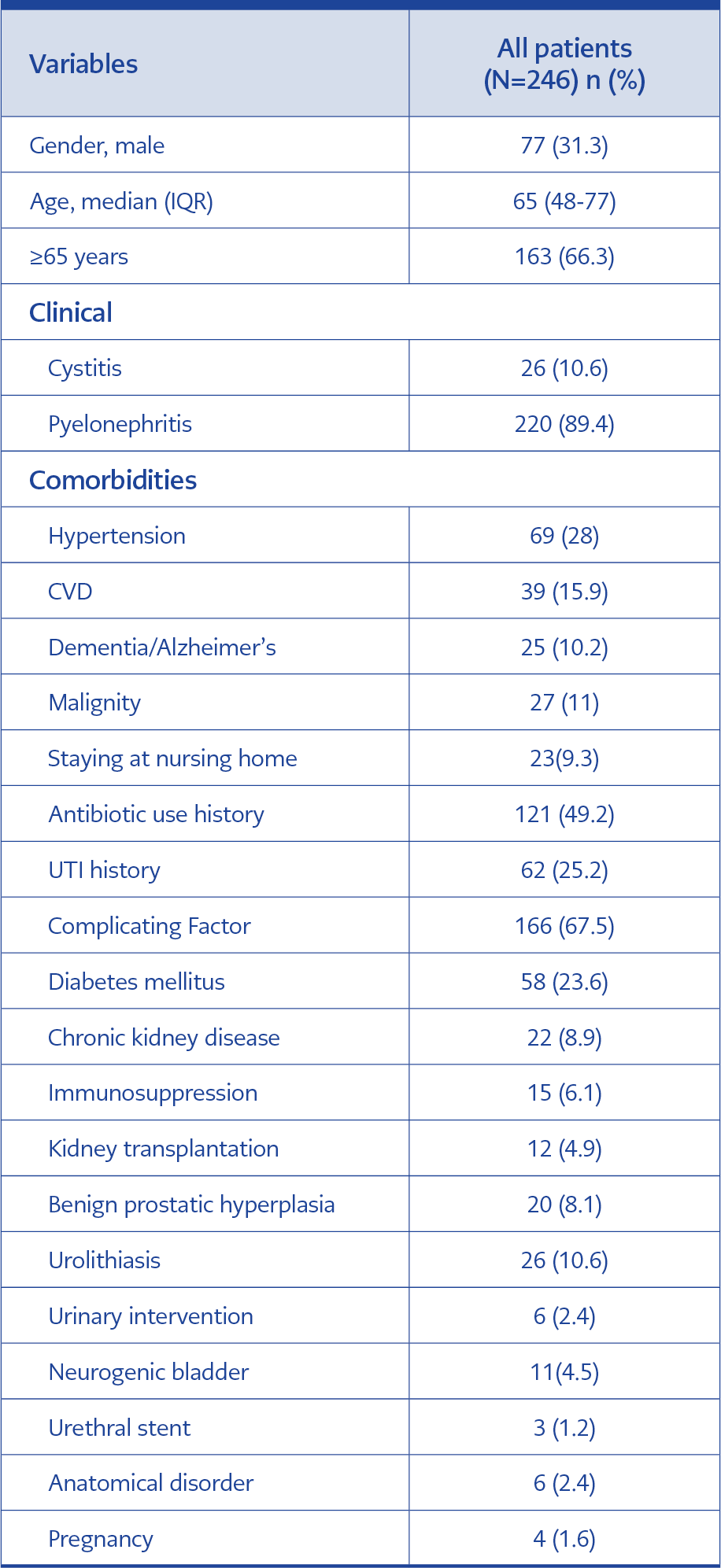
A total of 246 patients with CA-UTI were included in the study, of whom 68.7% were female. Of the patients, 166 (67.5%) were defined as having complicated UTIs and 80 (32.5%) as having uncomplicated UTIs. The most common complicating factors were diabetes mellitus (23.6%), urolithiasis (10.6%), and chronic kidney disease (8.9%). The demographics and complicating factors of the patients are presented in Table 1.
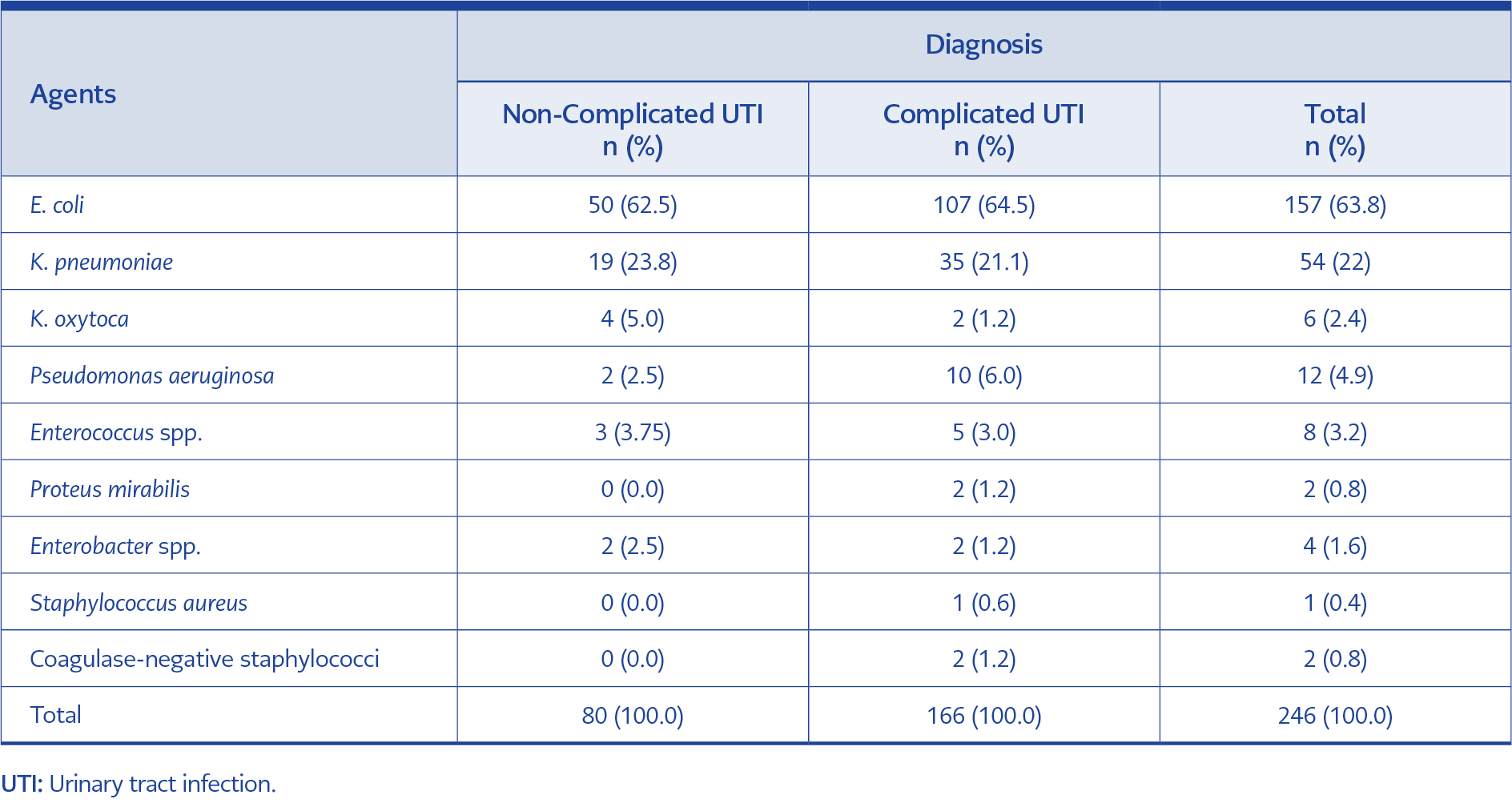
In the patients’ urine cultures, the most frequently isolated microorganism was E. coli, with a rate of 63.8%, and the second most frequently isolated
microorganism was K. pneumoniae, with a rate of 22%. Table 2 summarizes the examination of microorganisms according to diagnoses.
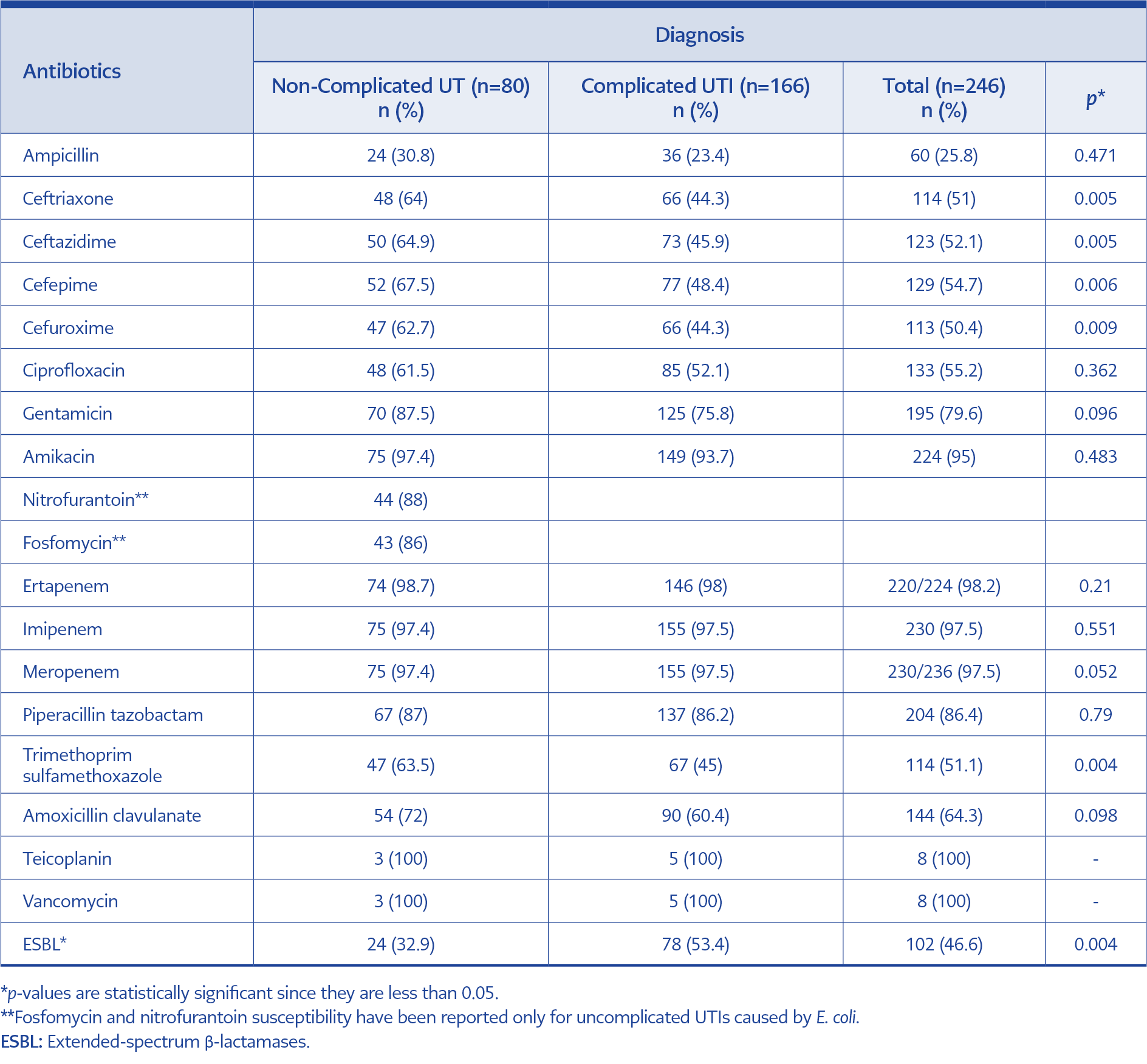
Table 3. Antibiotic susceptibility rates of agents isolated in non-complicated UTI and complicated UTI.
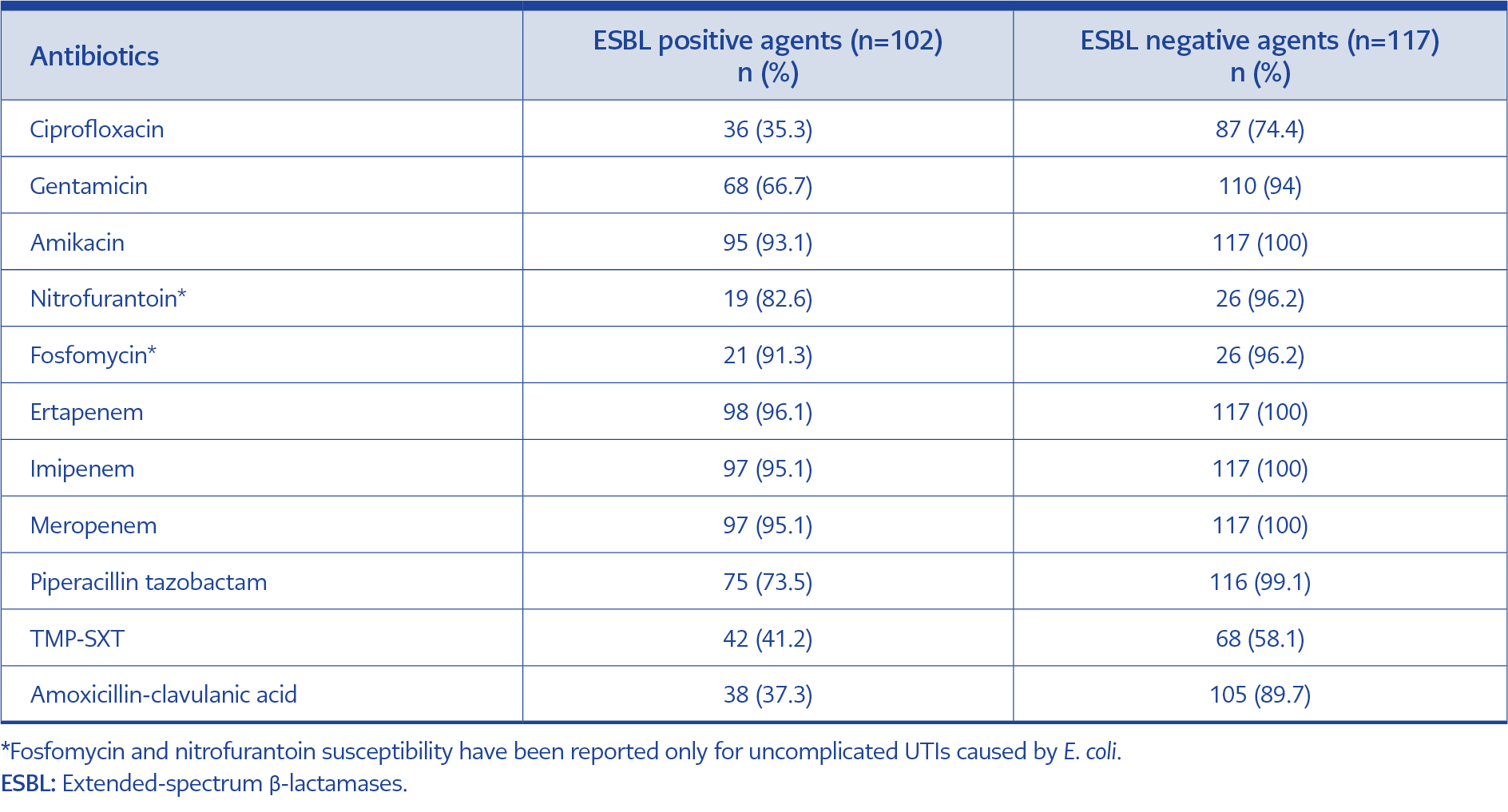
Sensitivity to the cephalosporin (ceftriaxone, ceftazidime, cefepime, cefuroxime) and trimethoprim-sulfamethoxazole (TMP-SXT) was observed to be low in the complicated UTI group (p=0.005, p=0.006, p=0.006, p=0.009, p=0.04, respectively). A total of 219 isolates of E. coli, Klebsiella spp., and Proteus spp. were examined regarding ESBL production and 102 (46.6%) samples were ESBL-positive. ESBL positivity was detected in 47.1% of E. coli isolates, 40.7% of Klebsiella pneumoniae isolates, 83.3% of Klebsiella oxytoca isolates, and 50% of Proteus mirabilis isolates. ESBL-producing microorganisms were higher (53.4%) in the complicated UTI group (p=0.04) (Table 3). The antibiotic susceptibility of ESBL-producing agents was 96.1% to ertapenem, 95.1% to imipenem-meropenem, 93.1% to amikacin, 91.3% to fosfomycin, 82.6% to nitrofurantoin, 73.5% to piperacillin-tazobactam, 66.7% to gentamicin, 41.2% to TMP-SXT, 37.3% to amoxicillin-clavulanic acid, and 35.3% to ciprofloxacin. The antibiotic susceptibility rates of ESBL-producing agents were quite low compared to non-ESBL-producing agents (Table 4).
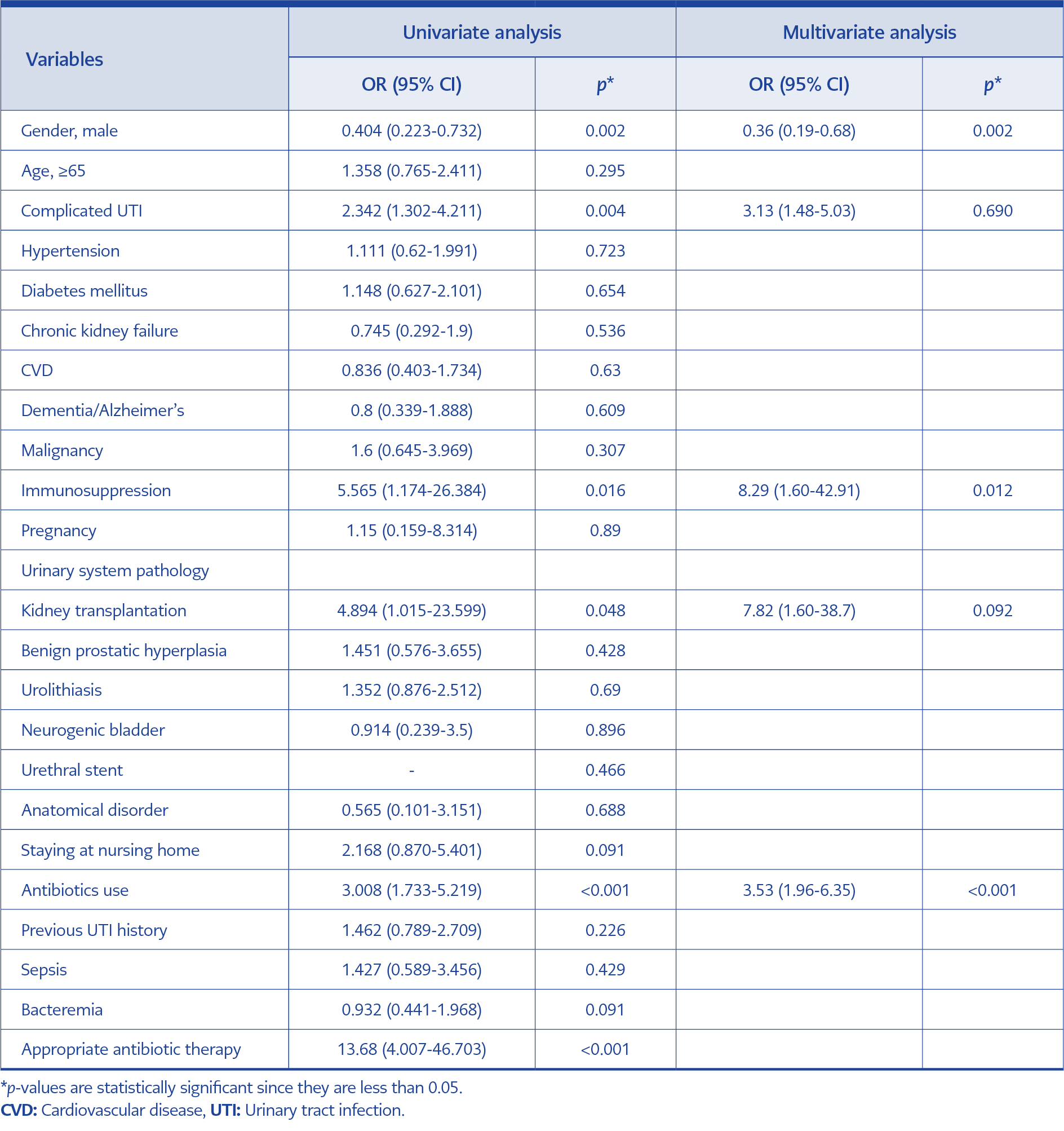
Table 5. Comparison of clinical and demographic characteristics of patients according to ESBL production with univariate and multivariate analysis.
ESBL positivity was significantly higher in males (62.1%) (p=0.02), in patients diagnosed with complicated UTI (53.4%), in patients with immunosuppression (81.8%) (p=0.16), in patients with a history of kidney transplantation (80%) (p=0.48), and in those with a history of antibiotic use (60.4%) (p<0.001). When the rates of bacteremia and sepsis were analyzed between ESBL-positive and ESBL-negative groups, no significant difference was found ([24.6%-26%, p=0.853] and [11.8%-8.5%, p=0.429], respectively). It was observed that the empirical treatment was ineffective in 26.5% of the ESBL-positive group and 2.6% of the ESBL-negative group (p<0.001). Five variables of gender, complicated UTI diagnosis, immunosuppression, history of kidney transplantation, and history of antibiotic use, found to be significant by univariate analysis of risk factors for ESBL-producing agents, were analyzed by multivariate analysis. According to this analysis, male gender (p=0.002), immunosuppression (p=0.012), and a history of antibiotic use (p<0.001) were independent risk factors for ESBL-producing agents (Table 5).
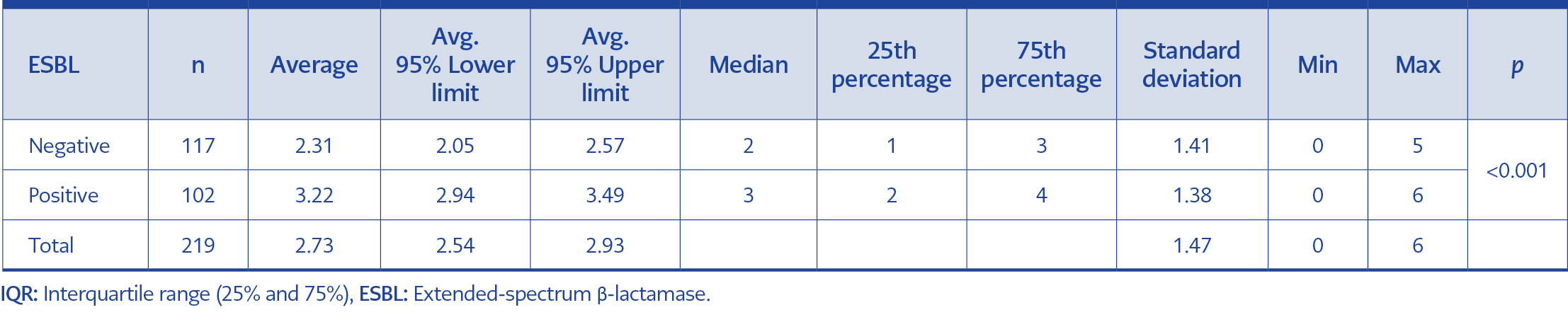
The variables were analyzed using receiver operating characteristics (ROC) analysis to demonstrate how the combination of risk factors and complicating factors for resistant infection affects the risk ratio for ESBL-producing agents. The risk factors evaluated in the ROC analysis compiled from the literature and international guidelines were the following: male gender, being ≥65 years old, diabetes mellitus, presence of malignancy, immunosuppression status, presence of urinary pathology, history of staying in a nursing home, history of antibiotic use, history of UTI (7,8). As a result of the analysis, it was tried to determine the area under the curve and the threshold factor number for the ESBL-producing agent. While the median number of variables was 2 (interquartile range [IQR]:1-3) in patients who were isolated non-ESBL-producing agents, it was 3 (IQR:2-4) in patients who were isolated ESBL-producing agents. According to the results of these tests, ESBL-producing agents were isolated at a low rate in patients with ≤ 2 risk factors, but the rate was high in patients with ≥ 3 risk factors (Table 6).
Discussion
Urinary tract infections, a critical cause of morbidity and mortality, are among the most common infections globally and in our country (9). Antibiotic resistance rates in microorganisms that cause urinary system infections have increased and become a severe health problem worldwide (10). Therefore, identifying risk factors for resistant microorganisms in patients diagnosed with UTIs and efficiently arranging treatment regimens would reduce morbidity and mortality.
E. coli is the most frequently isolated agent in both hospital-acquired and community-acquired UTIs, followed by K. pneumoniae from other Enterobacteriaceae spp. (11-13). In our study, the rates of E. coli and Klebsiella spp. strains were close to 90%. Knowing the resistance rates of these agents in CA-UTIs is very important for physicians in choosing the most appropriate empirical treatment for patients and rational use of antibiotics. The optimal treatment decision should be made by considering local resistance rates and the presence of risk factors for the development of resistant infection. UTI guidelines emphasize that if the local resistance rate against an antibiotic is higher than 10-20% in the population, that agent should not be preferred in empirical treatment. Previous studies on UTIs from our country have shown the highest resistance rates are against ampicillin, amoxicillin-clavulanic acid, TMP-SXT, ciprofloxacin, and cephalosporins (11, 14, 15). We found the highest resistance rates were in ampicillin (77.2%), TMP-SXT (48.9%), cephalosporins (>50%), and ciprofloxacin (44.8%). These agents are far from being an empirical treatment option for our country because their resistance rates exceed 40% within both the uncomplicated and complicated UTI groups, although lower in the uncomplicated group. In our study, the rate of ESBL-producing agents was 46.6%.
Several studies revealing the increase in ESBL rates in Enterobacterales species emphasize that the increase is not only in healthcare-associated infections but also in community-acquired UTIs (16,17). The increase in ESBL positivity rates reported from Turkey is particularly striking. ESBL-positivity in UTIs was 5-12% in the early 2000s in Turkey, while it was detected between 38-42% in the SMART study performed between 2011 and 2012 (12). In 2021, Kayaaslan et al. found ESBL positivity at 57.7% in community-acquired pyelonephritis (18); in our study, the rate of ESBL-positive CA-UTI was 46.6%. These high rates may be because of the high number of patients diagnosed with complicated UTI and pyelonephritis in our study, as in the study of Kayaaslan et al.
In line with previous studies, we demonstrated that the ESBL-positivity was higher in patients diagnosed with complicated UTIs than those with uncomplicated UTIs (19). However, this is also a result of inappropriate use and excessive consumption of antibiotics. Many international organizations, such as the Organization for Economic Cooperation and Development (OECD) and the World Health Organization (WHO), have reported that antibiotic resistance is high in Turkey (20, 21). Resistance rates against antibiotics are higher when the causative agent is ESBL-producing, and resistance to broad-spectrum antibiotics can also be observed (22). In our study, the agents with the closest resistance rates in ESBL-producing and non-ESBL-producing species were nitrofurantoin, fosfomycin, amikacin, and carbapenems (16, 23). Various studies stated that these agents could be preferred empirically in people with risk factors to have infections by resistant microorganisms (23). However, as shown in our study, our options for empirical treatment are quite limited, even in patients with no risk factor for developing infection by a resistant agent because of the increased resistance rates in CA-UTI agents.
Many studies have been conducted to determine the risk factors for ESBL-producing microorganisms. History of antibiotic use, history of UTI, urinary catheterization, advanced age, underlying diseases, and anatomical and functional disorders of the urinary system are prominent risk factors (22). When we compared ESBL-positive and negative groups, male gender, history of antibiotic use, and immunosuppression were determined as independent risk factors for developing infection by ESBL-positive agents. Univariate analysis showed that male gender, immunosuppression status, presence of complicating factors, history of kidney transplantation, and antibiotic use were significantly higher in the ESBL-positive group, which aligns with the literature (23-26). Previous studies generally associated ESBL-positive agents and high antibiotic resistance rates with hospital-acquired or healthcare-associated infections; however, it should be noted that they now also have a significant share in CA-UTIs (27).
In our study, empirical treatment change was statistically significantly higher in patients who were isolated ESBL-producing agents. This result revealed that we could not identify the risk factors for the ESBL-producing agents and initiate appropriate empirical treatment. Similarly, a study by Yang et al. showed that the success of empirical treatment was low in the patient group in which ESBL-producing agents were isolated, and the associated hospital stay and cost rates were high (28).
When nine variables of male gender, age ≥65 years, diabetes mellitus, presence of malignancy, immunosuppression status, presence of urinary pathology, history of staying in a nursing home, history of antibiotic use, and history of UTI were included in the analysis, regardless of being statistically significant or not, we concluded that patients having less than two risk factors could be administrated empirical treatment based on the prediction that a non-ESBL-producing agent would be isolated. For patients with three or more factors, empirical treatment should be administered based on the prediction that the agent could produce ESBL (Table 6). In our study, risk factors of male gender, complicated UTI diagnosis, history of immunosuppression, history of kidney transplantation, and history of antibiotic use were statistically significantly higher in the ESBL-positive group. Therefore, the possibility of an ESBL-positive agent should be considered in patients having these risk factors, and vice versa in patients not having, when choosing empirical treatment (Table 5). We found that male gender, immunosuppression, and a history of antibiotic use were independent risk factors for ESBL-producing agents. The risk of ESBL-producing agents increased 8.2 times in patients with immunosuppression and 3.5 times in patients with a history of antibiotic use.
By using quite narrow criteria, such as excluding antibiotic usage within the last six months, to determine community-acquired urinary tract infections, we could independently identify risk factors for resistant microorganisms. However, we are aware that the results may have been influenced by the low number of patients with cystitis and the high number of those diagnosed with complicated urinary tract infections. Studies involving more homogeneous groups are needed to identify risk factors for urinary tract infections caused by resistant microorganisms.
In conclusion, the resistance rates in our study are quite high. We found that male gender, history of antibiotic use and immunosuppression status were independent risk factors for ESBL positivity in patients with community-acquired urinary tract infections. The higher the number of risk factors, the greater the risk of ESBL positivity in patients.