Introduction
Healthcare-associated infections (HAIs) and antimicrobial resistance (AMR) represent major threats to global health. The global increase in AMR is primarily attributed to unnecessary or inappropriate use of antibiotics in humans and animals (1). Antibiotics, unlike other drugs, are a valuable resource that requires preservation for future generations. While the discovery of antibiotics has significantly extended human life expectancy, the lack of new antibiotic groups in recent years is concerning. The effective use of existing antibiotics is becoming increasingly limited due to rising AMR.
Mortality and morbidity caused by HAIs are much higher than those of other infectious diseases (IDs), and the number of deaths associated with AMR is increasing. It is estimated that there have been approximately 5 million deaths associated with bacterial AMR in 2019, including 1.3 million deaths attributable to AMR (2). Projections suggest that if current trends persist, AMR could be responsible for up to 10 million deaths annually by 2050, surpassing non-communicable diseases and becoming the leading cause of mortality worldwide (3,4).
The World Health Organization (WHO) developed the Access, Watch, and Reserve (AWaRe) classification to support antimicrobial stewardship (AMS) by categorizing antibiotics according to their antibacterial spectrum and impact on AMR. Antibiotics in the Access group pose a low risk for AMR and are recommended as first- and second-line treatments for common IDs. Watch group antibiotics are broader-spectrum agents with a greater risk of driving AMR and should be used in infections that cannot be treated with Access antibiotics. Reserve antibiotics serve as last-line options for severe infections caused by multidrug-resistant bacteria that cannot be managed by other medications. The WHO recommends that at least 60% of total antibiotic use should come from the Access group for combating AMR (5).
Antimicrobial stewardship programs aim to optimize antibiotic use, thereby improving patient outcomes and preventing adverse effects, the selection of AMR, and unnecessary costs associated with antimicrobials. Monitoring antimicrobial consumption and providing feedback are key strategies of AMS programs (6). Point prevalence surveys (PPSs) offer a standard methodology for assessing antimicrobial consumption and the prevalence of HAIs in hospitals. Data generated from PPSs are used to evaluate quality indicators, monitor AMS and infection prevention and control (IPC) programs, and support data-driven decision-making in healthcare services (7).
In this study, we aimed to evaluate both the quantitative (rate of antibiotic consumption by AWaRe category) and qualitative (appropriateness of antibiotic use) aspects of antimicrobial prescribing at our tertiary-care hospital using a point prevalence survey methodology.
Materials and Methods
Study Design and Settings
Dokuz Eylül University Research and Training Hospital is a tertiary-care center with 1100 beds located in İzmir, Türkiye. The Infection Prevention and Control Committee was established in 1992, making it one of the first hospitals in Türkiye to establish such a committee. Since 2005, PPSs for HAIs and antimicrobial consumption have been conducted twice annually, in January and June, as part of IPC activities. These surveys were suspended after June 2019 due to the COVID-19 pandemic and were resumed in June 2023.
Prevalence Survey and Data Collection
On June 16, 2023, training was provided to the IPC nurses, Infectious Diseases and Clinical Microbiology (IDCM) residents, and Medical Microbiology residents on the PPS methodology and completion of the data collection form. All hospitalized patients were included, except those in the hemodialysis unit, emergency department, and other outpatient care units. Patients admitted after 08:00 a.m. on the survey day were not enrolled.
The survey was conducted on June 19–20, 2023. Data were collected using the standardized PPS form across six intensive care units (ICUs) (Anesthesiology ICU, Internal Medicine ICU, Thoracic and Cardiovascular Surgery ICU, Cardiology ICU, Neonatal ICU, and Pediatric ICU), 17 medical departments (Nephrology, Gastroenterology, General Internal Medicine, Endocrinology, Rheumatology, Oncology, Hematology, Geriatrics, Pediatrics, IDCM, Neurology, Physical Therapy and Rehabilitation, Dermatology, Pulmonology, Palliative Care, Psychiatry, and Child Psychiatry), and 11 surgical departments (General Surgery, Orthopedics and Traumatology, Neurosurgery, Cardiovascular Surgery, Thoracic Surgery, Ophthalmology, Otorhinolaryngology, Plastic and Reconstructive Surgery, Pediatric Surgery, Urology, and Obstetrics and Gynecology).
In addition to demographic data, information regarding intrinsic and extrinsic infection risk factors, microbiological findings, and antimicrobial consumption was recorded. Data sources included nursing observation charts, the hospital information management system, and the microbiology laboratory.
Appropriateness of Antimicrobial Usage
Antimicrobial consumption was evaluated both quantitatively and qualitatively at the hospital-wide and unit-specific levels. For the quantitative evaluation, the antimicrobial consumption rate was calculated as the proportion of patients receiving antibiotics, with the numerator being the number of patients on antibiotics and the denominator being the total number of patients included in the survey. Additionally, the median duration (in days) of antibiotics being administered during the PPS was determined. Antibiotics were categorized according to the WHO AWaRe classification into Access, Watch, and Reserve groups, and their distribution was analyzed by hospital and departments (8).
For the qualitative evaluation, the appropriateness of antibiotic therapy and its duration, de-escalation based on culture results, and adherence to surgical prophylaxis protocols were assessed. Point prevalence survey forms were reviewed by an experienced IDCM specialist to assess the indications and the appropriateness of use.
Infections not present or incubating at the time of hospital admission and developed 48–72 hours after admission were classified as HAIs. Patients were also considered to have HAIs if they met any of the following criteria:
Hospitalization for more than two days within the past 90 days,
Receipt of outpatient treatments such as hemodialysis or chemotherapy,
Residence in a long-term care facility or nursing home,
Receipt of intravenous drug therapy, wound care, or private nursing care at home.
Antibiotics administered within 30–60 minutes prior to a surgical procedure and discontinued within 24 hours were considered appropriate surgical prophylaxis. Continuation of antibiotics beyond 24 hours postoperatively was recorded as inappropriate surgical prophylaxis. Prophylactic antibiotic use for non-surgical indications was classified as medical prophylaxis. The appropriateness of the antibiotic choice and duration was assessed according to the hospital’s local antibiotic guidelines. Antibiotic administration without a clear or documented indication was classified as inappropriate use.
The hospital’s local antibiotic guidelines were developed by a multidisciplinary team coordinated by the Department of IDCM. The Rational Antibiotic Use Team, a subgroup of the hospital’s IPC Committee, is responsible for regularly updating empirical and targeted antimicrobial treatment algorithms and strategies. These updates are based on patterns of AMR and adhere to national and international guideline recommendations.
This PPS was conducted in June 2023 as part of routine IPC activities at our hospital. In 2025, we re-analyzed the data with the aim of sharing our findings in a scientific publication to support AMS efforts in Türkiye. Prior to this analysis and manuscript preparation, ethical approval was obtained from the Non-Interventional Ethics Committee of Dokuz Eylül University, which granted it on May 14, 2025, under reference number 2025/16-35.
Statistical Analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS), version 29.0 (IBM Corp., Armonk, NY, USA). Categorical variables were summarized as numbers and percentages, and comparisons were made using Pearson’s χ² test or Fisher’s exact test, as appropriate. The distribution of continuous variables was assessed by histogram inspection, skewness and kurtosis values, and the Kolmogorov-Smirnov or Shapiro-Wilk tests. As continuous variables were not normally distributed, they were expressed as median and interquartile range (IQR), and comparisons were performed using the Mann-Whitney U test. A p-value of <0.05 was considered statistically significant.
Results
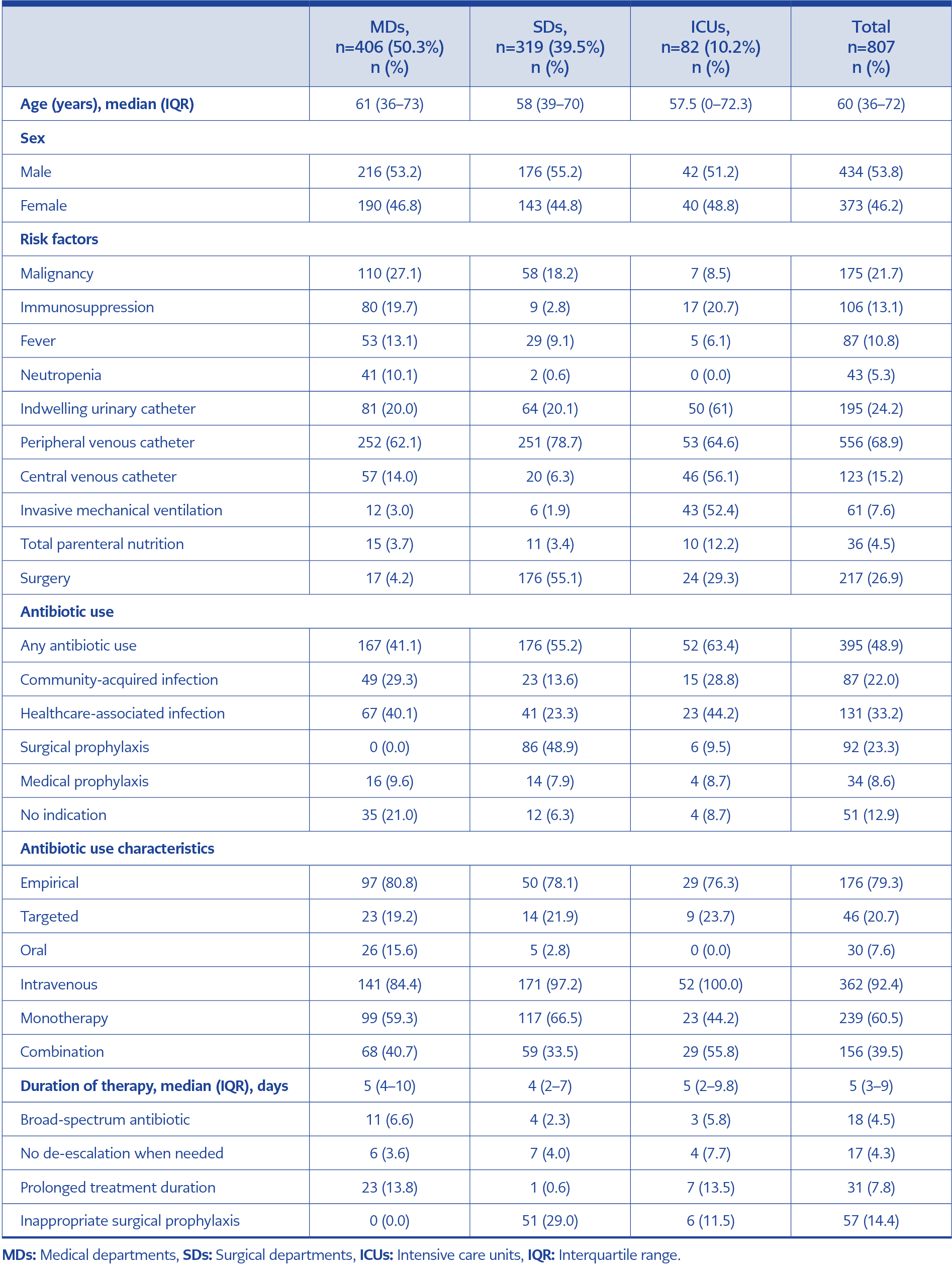
Table 1. Demographic characteristics, risk factors, and antibiotic use data of patients included in the point prevalence survey, stratified by hospital units.
A total of 807 patients were included in the study: 406 (50.3%) from medical departments, 319 (39.5%) from surgical departments, and 82 (10.2%) from ICUs. The median age of the patients was 60 years (IQR, 36–72), and 53.8% were male. The overall antibiotic use rate was 48.9% (395/807), which was significantly higher in patients aged ≥65 years compared to those aged 18–64 years (56.5% vs. 47.3%, p=0.015) and those under 18 years (56.5% vs. 33%, p<0.001). Patient demographics, risk factors, and antibiotic use characteristics are presented in Table 1.
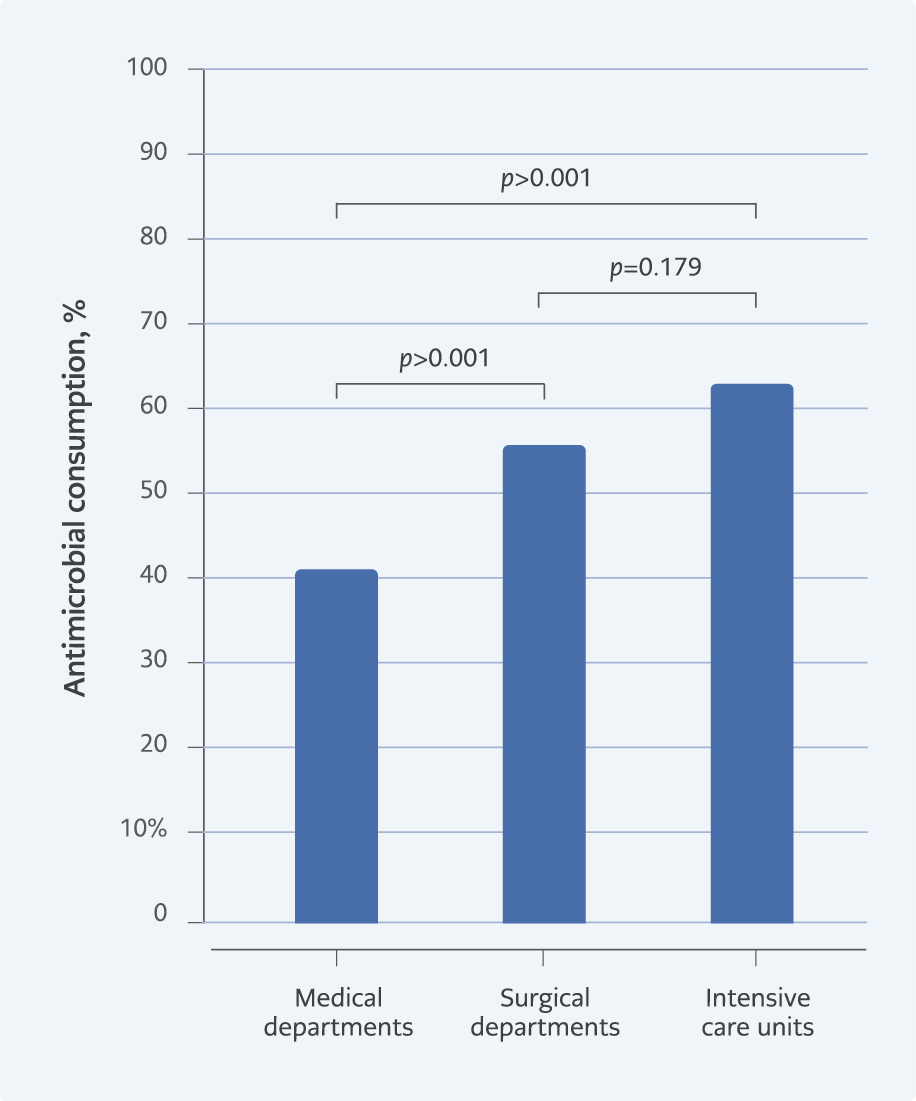
The antibiotic consumption rate was 63.4% in intensive care units, 55.1% in surgical departments, and 41.6% in medical departments. Antibiotic use was significantly lower in medical departments compared to surgical departments (p<0.001) and ICUs (p<0.001) (Figure 1). The units with the highest antibiotic consumption were Anesthesiology ICU (94.4%), Internal Medicine ICU (88.9%), IDCM ward (87.5%), Thoracic and Cardiovascular Surgery ICU (80%), and Pulmonology ward (75.8%).
Blood cultures were positive in 11.0% (n=89) of patients. The most frequently isolated pathogens were coagulase-negative staphylococci, Klebsiella pneumoniae, and Candida spp., respectively. The results of blood cultures and resistance data for clinically important microorganisms are presented in Table 2. These include third-generation cephalosporin resistance in Escherichia coli (40%), carbapenem resistance in K. pneumoniae (66.7%), Pseudomonas aeruginosa (50%), and Acinetobacter baumannii (100%), as well as ceftazidime-avibactam resistance in K. pneumoniae (22.2%) and vancomycin resistance in enterococci (28.6%).
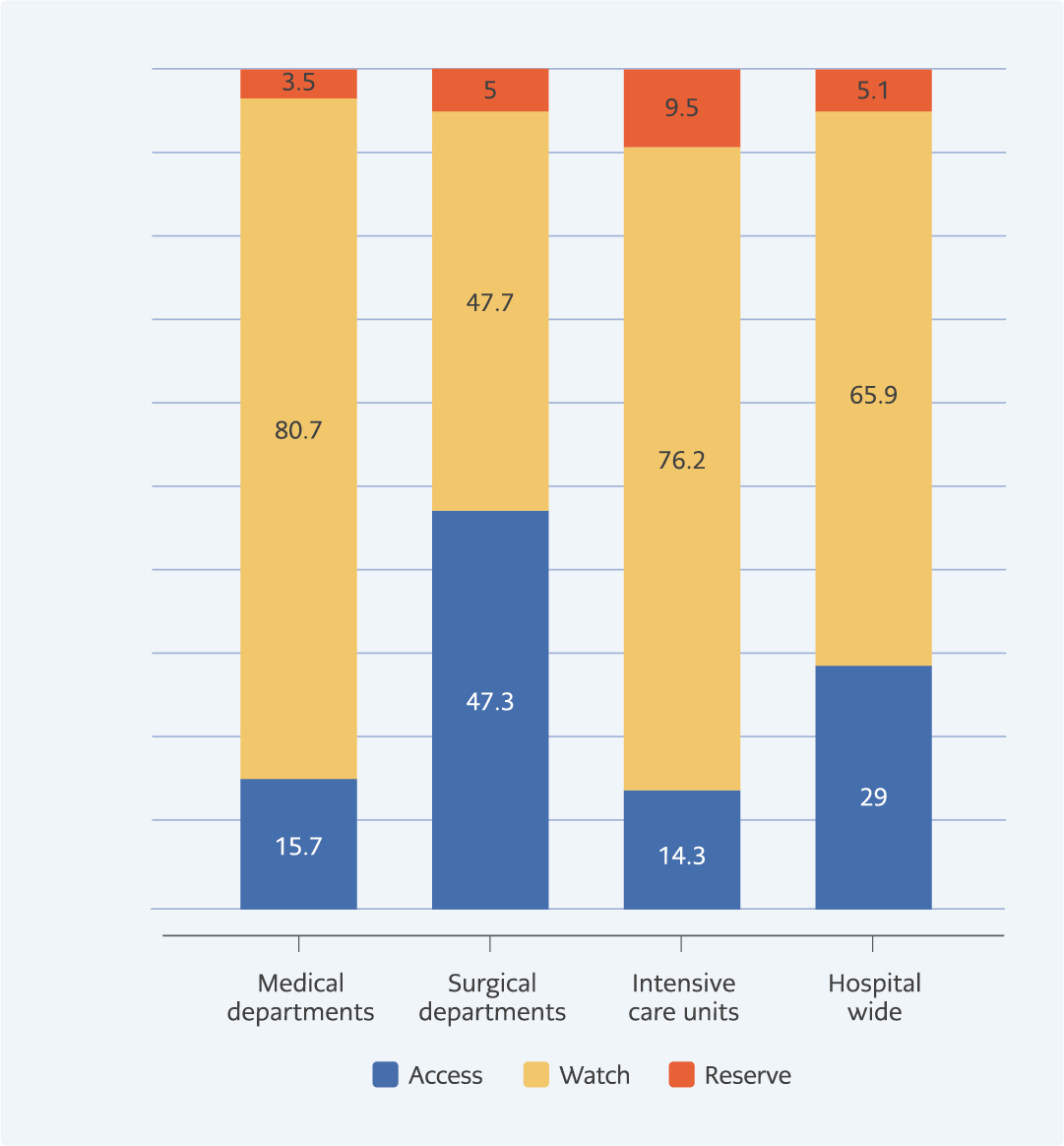
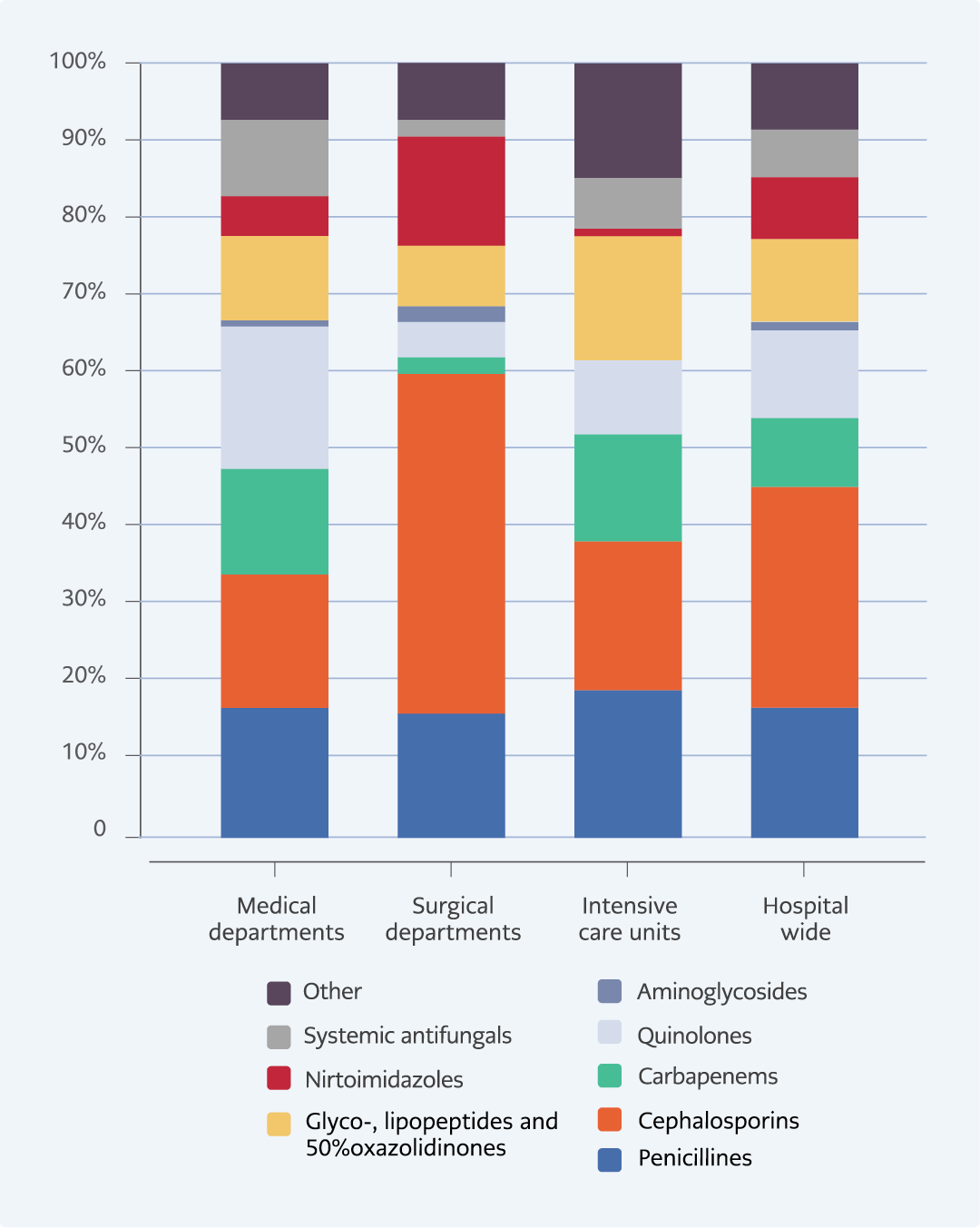
Cephalosporins (20.3%), penicillins (12.4%), and quinolones (8.3%) were the most frequently used antibiotic groups. The most commonly prescribed agents were piperacillin-tazobactam (10.5%), cefazolin (7.9%), ceftriaxone (6.8%), and meropenem (5.9%). According to the WHO AWaRe classification, 29% of prescriptions belonged to the Access group, 65.9% to the Watch group, and 5.1% to the Reserve group. Access antibiotics were predominantly used in surgical departments, Watch group agents in medical departments, and Reserve group agents in ICUs. Unit-specific usage patterns are presented in Figures 2 and 3.
Antibiotics were used for therapeutic purposes in 222 patients (27.5%). Of these, 79.3% were empirical and 20.7% were targeted treatments. Infections were healthcare-associated in 60.4% and community-acquired in 39.6%. In 51 patients (12.9%), there was no clear indication for antibiotic use. Broad-spectrum empirical therapy was started in 18 patients (4.5%), and no appropriate de-escalation was made in 17 patients (4.3%). Treatment duration was longer than recommended in 31 patients (7.8%).
Surgical prophylaxis was given in 92 patients (23.3%), and medical prophylaxis in 34 patients (8.6%). Cefazolin was the most commonly used agent for surgical prophylaxis. Although the correct antibiotic, dose, and timing were used, 61.9% of surgical prophylaxis cases exceeded 24 hours and were considered inappropriate.
Discussion
The prevalence of antimicrobial use was high in our hospital at 48.9%. A systematic review and meta-analysis from Türkiye, which evaluated 17 studies conducted between 2004 and 2020, reported a median of antimicrobial use prevalence of 45% (IQR, 36–65) (9). Point prevalence surveys conducted in various countries have shown considerable variation in antimicrobial use. Antimicrobial use was generally lower in high-income countries, with reported rates of 27.1% in Belgium, 29.2% in Japan, 32% in Switzerland, 33.5% in Canada, and 47.3% in Italy (10-14). In contrast, a multinational PPS study from Latin America reported a prevalence of 54.6% (15), while studies from African countries showed a wide range between 46% and 73.7% (16-20). The prevalence reached 75% in Pakistan (21) and 73.5% in Bangladesh (22). Lower antibiotic use in high-income countries is attributed to strong national and institutional AMS programs. In contrast, in low- and middle-income countries, the lack of institutional guidelines or treatment algorithms, limited surveillance and feedback on antimicrobial use, inadequate microbiological diagnostics, and insufficient infrastructure and workforce negatively affect antimicrobial prescribing practices.
In our hospital, 79.3% of therapeutic antibiotic use was empirical, and 60.4% of these cases were HAIs. Cephalosporins (20.3%), penicillins (12.4%), and quinolones (8.3%) were the most used groups, and piperacillin-tazobactam was the most commonly prescribed antibiotic. During the study period, ampicillin-sulbactam was not available in the hospital pharmacy. As a result, piperacillin-tazobactam and third-generation cephalosporins were used more often when a β-lactam/β-lactamase inhibitor was indicated. A review of studies from Türkiye reported an empirical antibiotic use rate of 71%, with third-generation cephalosporins being the most frequently used group (9). In high-income countries, β-lactam/β-lactamase inhibitors are the most commonly used antibiotics (10,12-14), whereas in low- and middle-income countries, third-generation cephalosporins—especially ceftriaxone—are more widely preferred (15,17,18,20-22).
The WHO recommends that more than 60% of antimicrobial use should belong to the Access group according to the AWaRe classification, to tackle AMR (5). Only 29% of antibiotics in our hospital belonged to the Access group, while approximately 70% were in the Watch group and 5% in the Reserve group. The frequent use of Watch antibiotics in our hospital may be due to the high prevalence of AMR and the predominance of HAIs. Although this study did not include longitudinal AMR surveillance data, resistance data for clinically important bloodstream isolates obtained within the 7 days prior to the PPS were presented. These findings offer a representative snapshot of the local AMR situation during the survey period and support the interpretation of antimicrobial prescribing behaviors observed in the study.
In Türkiye, a national antibiotic restriction policy has been in place since 2003. Narrow-spectrum antibiotics, including penicillins, first-generation cephalosporins, aminoglycosides, and macrolides, can be prescribed by all physicians without restriction. Parenteral third-generation cephalosporins and quinolones can be prescribed by specialists but require approval from an IDCM specialist after 72 hours through a computerized pre-authorization system. For agents with broader spectra—such as anti-pseudomonal β-lactams, fourth-generation cephalosporins, carbapenems, anti- methicillin-resistant Staphylococcus aureus (MRSA) agents (vancomycin, daptomycin, linezolid), polymyxins, and novel agents like tigecycline or ceftazidime-avibactam—IDCM approval is required before administration. This national strategy is actively implemented in our hospital. However, we also emphasize that restriction-based policies alone are insufficient. A combination of restrictive and persuasive AMS strategies is necessary to improve prescribing practices and increase the use of Access group antibiotics. To date, no other study from Türkiye has been found that evaluates inpatient antibiotic consumption based on the WHO AWaRe classification.
The Global Point Prevalence Survey (Global-PPS Network) assessed antimicrobial use among adult inpatients from 664 hospitals across 69 countries. The findings demonstrated that antimicrobial use patterns varied by region and country income level. Access antibiotics were prescribed more frequently in Oceania and in Northern and Western Europe but were less commonly used in Southern and Eastern Europe, where Watch antibiotics predominated. The lowest use of Access antibiotics was observed in Central and Western Asia, with rates below 30%. When analyzed by income level, the proportion of Access antibiotics use was 45% in high-income countries, 33% in middle-income countries, and 62.8% in low-income countries (23). The higher percentage of Access use in high-income countries compared to middle-income countries may be attributed to more effective AMS programs, better implementation of IPC measures, and lower AMR rates. In contrast, the higher Access use in low-income countries, despite elevated AMR rates, is likely related to the limited availability of Watch and Reserve antibiotics.
According to our study, 43.9% of antimicrobial use was inappropriate. The most common reasons were the use of antibiotics without a clear indication, inappropriate surgical prophylaxis, and prolonged duration of antimicrobial therapy. A systematic review from Türkiye reported a median prevalence of inappropriate antimicrobial use of 36% (IQR: 26–41) in hospitals. Similar problems were identified, including the use of broad-spectrum antibiotics without indication, a combination of antibiotics with overlapping spectra, prolonged duration, and inappropriate surgical prophylaxis (9). In South Korea, a nationwide multicenter study found that 27.7% of cases involved inappropriate use, with surgical prophylaxis being the primary contributor (24). A national PPS study in the UK reported a 30.4% prevalence of inappropriate antimicrobial use for community-acquired infections, primarily due to deviation from guideline recommendations and prolonged duration (25). A study from Switzerland showed that in 60% of patients receiving prophylaxis, it continued unnecessarily, and 58% of therapeutic prescriptions required optimization, mainly due to unnecessarily extended treatment (12). In Tanzania, all antibiotic treatments were empirical, guideline compliance was only 45%, and 55% of patients received inappropriate empirical therapy (17). These findings suggest that the inappropriate use of antimicrobials is a significant global issue. Common themes include unnecessary use, inappropriate surgical prophylaxis, and excessively long treatment durations. These results highlight the universal need for AMS programs and emphasize the importance of implementing guideline-based practices at both national and institutional levels.
In our institution, IDCM specialists approve or initiate antibiotic therapy as part of the national restriction policy. Ongoing monitoring of antibiotic use is generally conducted by the primary physician. Infectious disease follow-up is usually re-initiated when culture results are available or if the patient’s condition worsens. In intensive care units, IDCM specialists are more regularly involved in patient management. However, limited IDCM staffing and high workload prevent daily follow-up for all patients, which may contribute to unnecessarily prolonged antibiotic use. These findings underscore the need for improved collaboration and stewardship mechanisms to support timely de-escalation and discontinuation of antibiotics.
This study has several limitations. As it was conducted in a single tertiary university hospital, the findings may not fully represent antibiotic use patterns across hospitals in Türkiye. The unavailability of ampicillin-sulbactam during the study period led to an increase in the use of piperacillin-tazobactam and ceftriaxone, which influenced the observed antibiotic distribution and limited the accuracy of assessing prescribing preferences. We could not assess the appropriateness of antibiotic use separately for the WHO Access, Watch, and Reserve groups, as some patients received combination regimens involving multiple AWaRe categories. The uneven distribution of cases among these groups further restricted comparative analysis. Further research should include larger sample sizes and standardized metrics for AWaRe-based appropriateness. To better understand antibiotic consumption trends in Türkiye, multicenter studies involving different geographic regions and types of hospitals are needed.
This study identified a high overall antibiotic use rate in the hospital (50%). Antibiotics were prescribed therapeutically in 55.2% of cases, prophylactically in 31.9%, and without indication in 12.9%. The high prevalence of HAIs and concerns about antimicrobial resistance contributed to the increased use of Watch group antibiotics. Inappropriate antimicrobial prescribing was most frequently associated with prolonged surgical prophylaxis, extended treatment durations, and empirical therapy without clear indications. To optimize antimicrobial use and mitigate the threat of AMR, targeted interventions are needed. These should focus on improving adherence to surgical prophylaxis guidelines, minimizing unnecessary treatment duration, and regularly updating institutional guidelines. These findings emphasize the critical role of effective AMS and IPC programs in optimizing antibiotic use, increasing Access group utilization in line with WHO recommendations, and preventing AMR in hospital settings.