Introduction
Hepatitis B virus (HBV) infection is an important public health problem worldwide. It is the most important cause of acute and chronic liver disease and hepatocellular cancer (1). Hepatitis B infection is diagnosed by the detection of HBsAg in the serum or plasma. Chronic hepatitis B (CHB) infection is defined as the persistence of inflammation in the liver for six months or longer. Early diagnosis and accurate assessment of liver damage are essential for evidence-based clinical treatment (2). According to current clinical practice, serum alanine aminotransferase (ALT) and HBV DNA levels, degree of necroinflammation in liver biopsy, and fibrosis stage can be used to determine treatment decisions and prognosis in patients with CHB (3). Liver biopsy remains the gold standard for the diagnosis of CHB. However, reasons such as the fact that biopsy is an invasive and laborious procedure, complications that may occur after the procedure, the inadequacy of the biopsy material for histological diagnosis, difficulties in repeating the biopsy, the need for an expert pathologist’s opinion and its high cost have led clinicians to search for noninvasive methods (4, 5, 6). For this purpose, serum biomarkers and transient elastography (FibroScan) among imaging techniques can be used (7). Biochemical markers include aspartate aminotransferase (AST), ALT, gamma-glutamyl transpeptidase (GGT), alkaline phosphatase (ALP), albumin, total bilirubin, cholesterols, platelets (PLTs), prothrombin time, international normalized ratio (INR), α2-macroglobulin, hyaluronic acid, apolipoprotein A1, metalloproteinase enzymes, transforming growth factor-beta 1 (TGF-β1), TGF-α can be used. The World Health Organization (WHO) recommends the AST-to-platelet ratio index (APRI) and fibrosis-4 (FIB-4) score as diagnostic biochemical markers for liver fibrosis (8).
In this study, the severity of fibrosis in liver needle biopsy of treatment-naive patients with CHB was compared with the APRI and FIB-4 scores in terms of sensitivity and specificity.
Materials and Methods
This was a single-center retrospective cohort study. This study complies with the Declaration of Helsinki and is approved by the Van Training and Research Hospital Clinical Research Ethics Committee with decision number 2023/13-04 on June 21, 2023.
Patients older than 18 years of age who were followed up with a diagnosis of CHB between 2018 and 2023 in the Infectious Diseases and Clinical Microbiology outpatient clinic of Van Training and Research Hospital between 2018 and 2023, who had not previously received treatment for hepatitis B disease, and who underwent liver biopsy were included in the study. Although biopsy was not required in some patients based on HBV DNA values, biopsy was performed in patients with military committee reports and long-term follow-up due to a family history of liver failure. Patients with concomitant acquired immunodeficiency virus (HIV), hepatitis C (HCV) virus, hepatitis D virus (HDV) infection, decompensated liver disease or hepatocellular malignancy at the time of diagnosis, alcoholic hepatitis, autoimmune hepatitis, hepatotoxic drug use, or insufficient liver biopsy samples were excluded.
The patients’ blood tests and liver biopsy results were obtained by retrospective scanning from the hospital automation system. Age, gender, AST, ALT, HBV DNA, bilirubin, albumin, INR, and AFP values, platelet counts, and liver ultrasonography (USG) findings before biopsy were recorded. Liver biopsies were evaluated based on the modified Ishak fibrosis score. The patients were divided into three groups according to the Ishak fibrosis score. Cases with stages 0-1 were grouped as having no fibrosis, cases with stages 2-3 as having mild fibrosis, and cases with stages 4-5-6 as having severe fibrosis. The histological activity index (HAI) at the end of the biopsy was expressed as numbers (1-14).
FIB-4 and APRI, as the noninvasive scores appropriate according to the blood tests performed in our hospital, were used. The FIB-4 score and APRI were calculated according to the following formulas:
FIB-4 Score= Age (years)×AST (U/L) / [PLT (109/L)×ALT1/2 (U/L)]
APRI=[AST (U/L) / (AST (Upper Limit of Normal) (U/L)] / Platelet Count (109/L)×100
The statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) 22.0 (IBM Corp., Armonk, NY, USA). In statistical analyses, the conformity of all measured variables to a normal distribution was evaluated using the Kolmogorov-Smirnov test. Continuous variables were expressed as median (minimum and maximum values) because they did not fit the normal distribution, whereas frequency (categorical) data were expressed as numbers and percentages (%). The Kruskal-Wallis test was used to compare continuous data between groups, and the Pearson chi-square test was used for categorical data. Receiver operating characteristic (ROC) analyses were performed to determine the cut-off point of the APRI and FIB-4 scores in terms of fibrosis, considering the liver biopsy results. The statistical significance was set as p<0.05.
Results
The median age of the 202 patients included in the study was 40 years (19-76), and 63.4% were male. HBV DNA was negative in 26 patients (12.9%), HBV DNA <2000 IU/mL in 30 patients (14.9%), HBV DNA 2000-20,000 IU/mL in 29 patients (14.3%), and HBV DNA >20,000 IU/mL in 117 patients (57.9%).
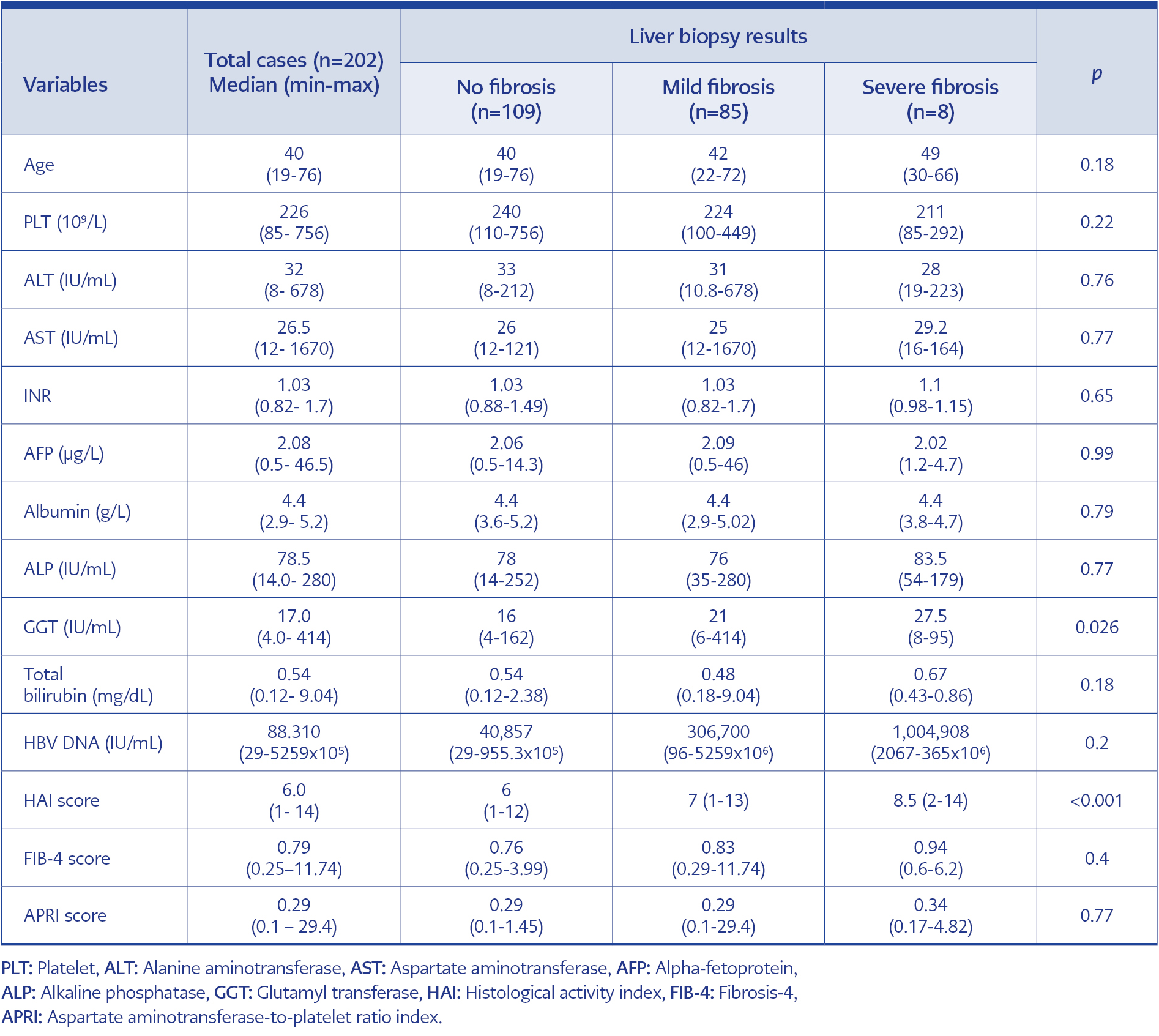
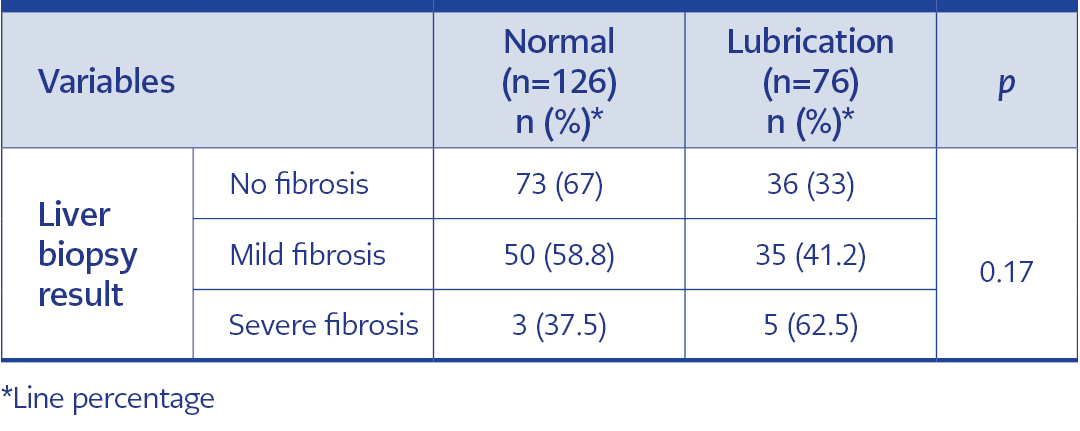
Table 1. Evaluation of laboratory values and clinical scores of all cases and case groups according to the liver biopsy results.
According to liver biopsy results, 109 (54.0%) patients had no fibrosis, 85 (42.1%) had mild fibrosis, and 8 (4.0%) had severe fibrosis. Regarding liver USG findings, 126 (62.4%) of the patients had normal USG findings, 55 (27.2%) had grade 1 adiposity, 15 (7.4%) had grade 2 adiposity, and six (3.0%) had coarse granular patterns. The median HAI score was 6.0 (1.0-14.0), the median FIB-4 score was 0.79 (0.25-11.74), and the median APRI score was 0.29 (0.10-29.40). The laboratory analysis results and clinical diagnosis scoring results of the patients are given in Table 1. When the laboratory data of the case groups were compared according to the liver biopsy results, there was a statistically significant difference between the groups in terms of the median GGT value, and GGT was highest in the severe fibrosis group and lowest in the non-fibrosis group (p=0.026). There were no significant differences between the groups in terms of other laboratory data (p>0.05) (Table 1). According to the liver biopsy results, there was no difference between the groups in terms of FIB-4 and APRI score medians (p=0.40 and p=0.77, respectively), but there was a significant difference in terms of HAI score (p<0.001) (Table 1).
While the liver USG findings were normal in 126 (62.4%) patients, 76 (37.6%) had fatty deposits. When pathologic USG findings were analyzed, grade 1 fatty deposits (72.4%) and grade 2 fatty deposits (19.7%) were the most common, and a coarse granular appearance was present in six cases (7.9%). The USG findings were normal in 37.5% of the patients with severe fibrosis, according to liver biopsy. However, there was no statistically significant difference in the USG findings between the groups (p=0.17) (Table 2).
When the cases were grouped according to HBV DNA levels and their distribution according to score groups was analyzed, there was no statistically significant difference in the distribution of HBV DNA groups in liver biopsy results and FIB-4 score groups (p>0.05). However, according to the APRI score in the HBV DNA groups, the frequencies of those with mild fibrosis were significantly different from the others (no fibrosis and severe fibrosis) (p=0.003).
When the correlation of the calculated clinical scores of the patients was evaluated, there was a statistically highly significant linear relationship between the HAI score and FIB-4 and APRI scores in the positive direction with weak strength (r=0.23 and p=0.001; r=0.19 and p=0.006, respectively). There was a moderate and highly significant linear relationship between FIB-4 and APRI scores (r=0.51 and p<0.001).
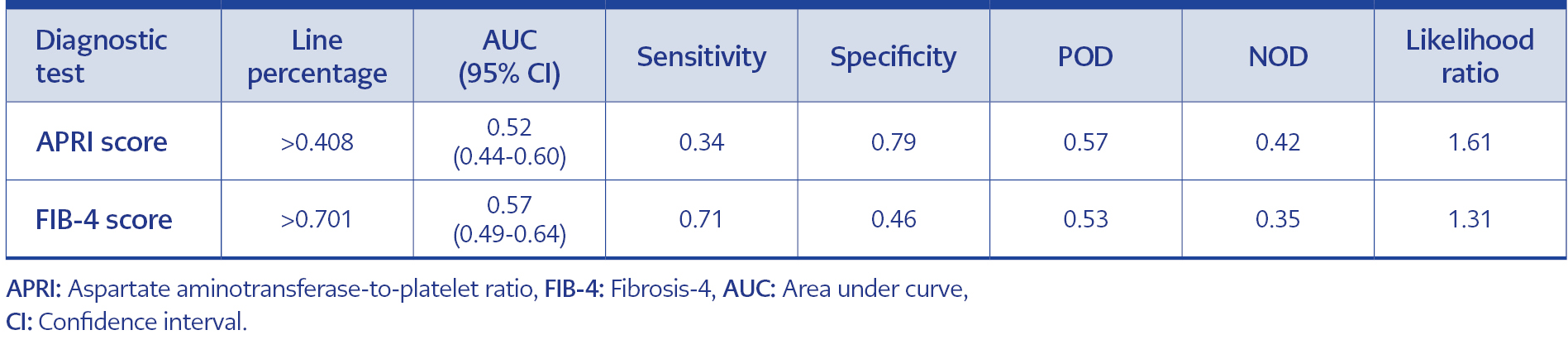
Table 3. Comparison of patients without fibrosis with those with fibrosis (mild fibrosis + severe fibrosis) according to liver biopsy.
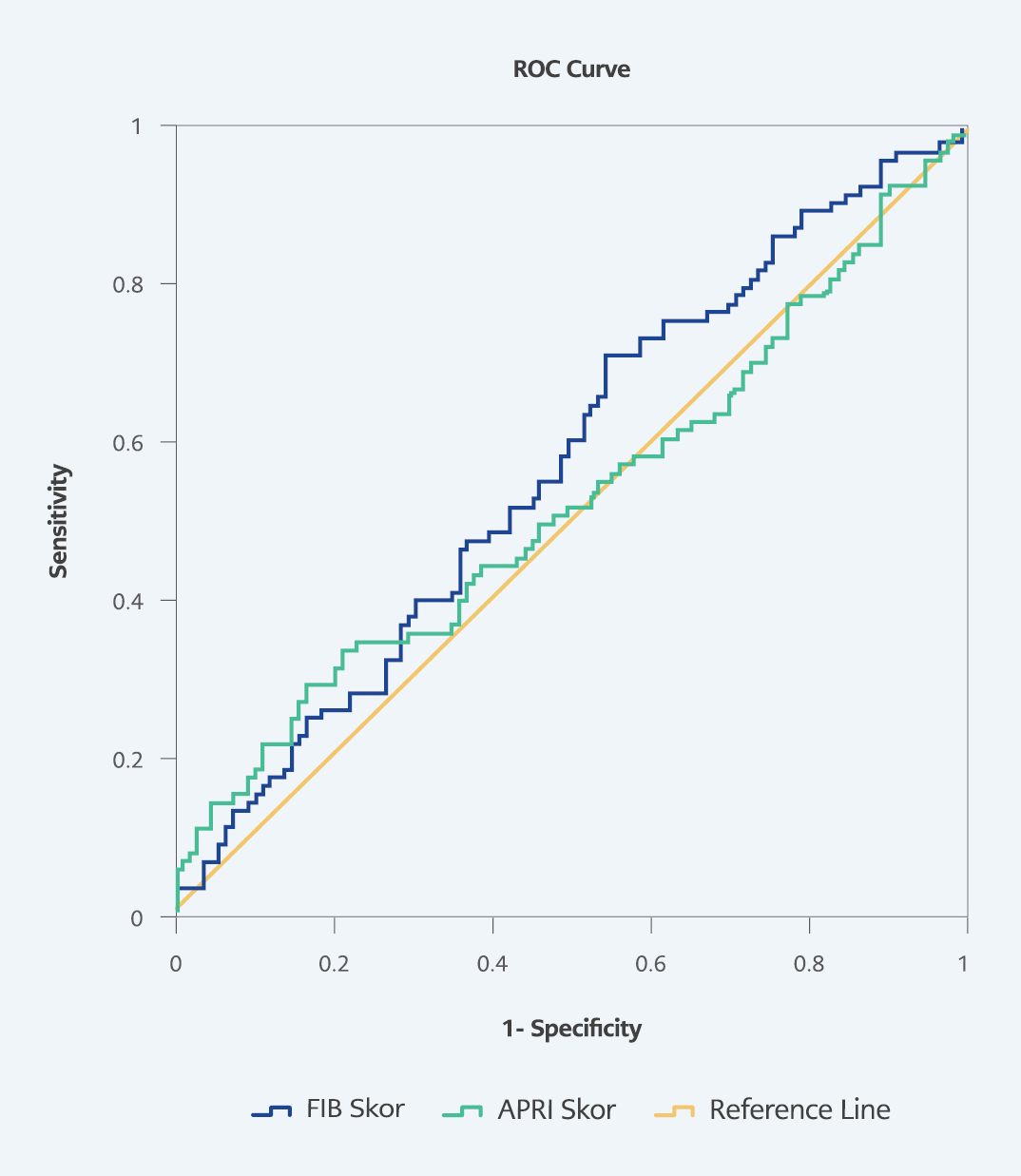
Figure 1. According to ROC analysis, the ability of FIB-4 and APRI scores to distinguish patients without fibrosis from patients with fibrosis (mild fibrosis + severe fibrosis) according to liver biopsy.
When the power of the APRI score in predicting the discrimination between “without fibrosis” and “with fibrosis (mild and severe)” was evaluated by ROC analysis considering the liver biopsy results of the patients, for APRI score >0.408 as the ideal cut-off point, sensitivity and specificity were found to be 34% and 79%, respectively. In the same situation, for the FIB-4 score when the cut-off point was >0.701, sensitivity and specificity were 71% and 46%, respectively (Table 3) (Figure 1).
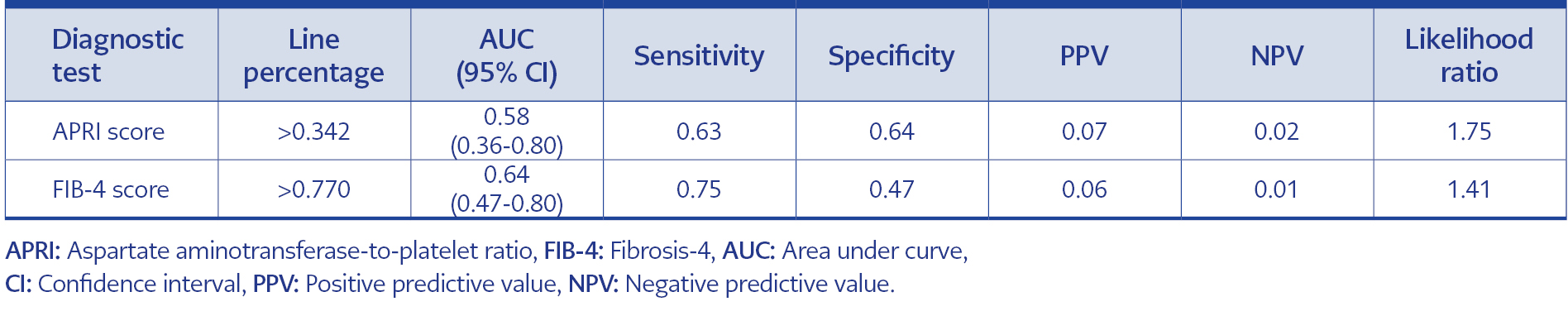
Table 4. Comparison of patients with no fibrosis and mild fibrosis with those with severe fibrosis according to liver biopsy.
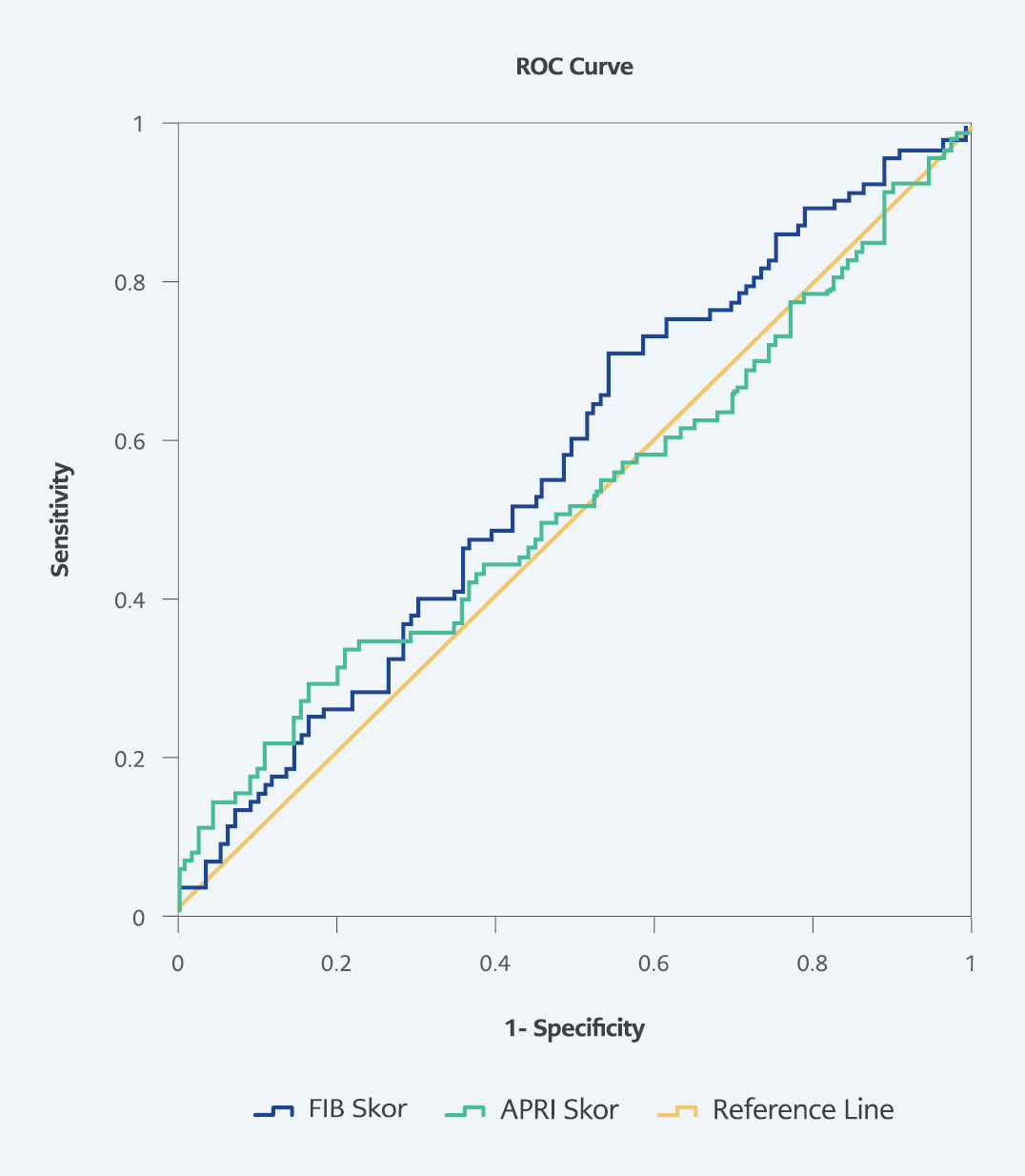
Figure 2. According to ROC analysis, the ability of FIB-4 and APRI scores to distinguish between patients without fibrosis and those with mild fibrosis + sever fibrosis according to liver biopsy.
When an APRI score >0.342 was taken as the ideal cut-off point to differentiate patients “without fibrosis and with mild fibrosis” from patients with “severe fibrosis” according to liver biopsy, the sensitivity and specificity were 63% and 64%, respectively. When the cut-off point for the FIB-4 score was >0.770, the sensitivity and specificity were 75% and 47%, respectively (Table 4) (Figure 2).
Although the area under the curve (AUC) ratios ranged between 52% and 64% in the ROC analyses, and the sensitivity ratios of the cut points calculated for FIB-4 were higher, the likelihood ratios of the cut points we found for the APRI score (1.61 and 1.75, respectively) were relatively better than the likelihood ratios of the cut points we found for FIB-4 (1.31 and 1.41, respectively).
Discussion
Liver fibrosis status is one of the main prognostic factors in determining the risk of the development of liver cirrhosis and hepatocellular carcinoma that may occur after chronic liver diseases (8). A liver biopsy is the gold standard for evaluating liver damage caused by HBV infection (9). However, liver biopsy carries the risk of representing only a very small portion of the entire liver (10). A biopsy specimen of sufficient length and size should be obtained to avoid this problem (3, 11). In addition to technical problems, liver biopsy requires an experienced pathologist and a well-equipped hospital, and the invasive nature of the procedure carries a risk of complications, such as hemorrhage, hemobilia, biliary colic, pneumothorax, and peritonitis, which may be rare but fatal.
All of the issues mentioned above limit the use of liver biopsy for the screening of liver fibrosis. Therefore, liver biopsy is not always the best and easiest option in clinical practice, and other easily applicable biomarkers are needed to assess liver injury. Currently, fibrosis determinant scores such as AST/ALT ratio, APRI, FIB-4, age-platelet (AP) index, Hui score, Lok score, Goteborg University cirrhosis index (GUCI), cirrhosis discriminant score (CDS), Zeng score can be calculated by using various serum biochemical markers (3, 12, 13). The World Health Organization (WHO) and many guidelines recommend APRI and FIB-4 scores as noninvasive diagnostic methods for liver fibrosis in chronic viral hepatitis and transient elastography (TE), which measures liver stiffness among imaging methods (9, 14-16).
In our study, when the laboratory data of the patient groups were compared according to the liver biopsy results, there was no significant difference between the groups in terms of laboratory data except the GGT value. GGT is an enzyme used to synthesize glutathione, an accepted biological indicator of hepatocellular damage. GGT may also be secreted by inflammatory cytokines during malignancy and inflammation. In previous studies, the relationship between fibrosis values and serum GGT levels was evaluated, and it was reported that there was a positive correlation with elevated GGT levels in the high-stage fibrosis group (17-20). Consistent with the literature, GGT levels were significantly higher in the group with high fibrosis scores and stages in our study.
When we compared APRI scores according to liver biopsy, they were higher in the group with severe fibrosis (0.34 [0.17-4.82]). When the patients were grouped according to liver biopsy fibrosis and evaluated by ROC analysis for an APRI score >0.342, which was obtained to differentiate patients with “no fibrosis and mild fibrosis” from patients with “severe fibrosis,” sensitivity and specificity were found to be 63% and 64%, respectively. To differentiate “no fibrosis” and “mild fibrosis and heavy fibrosis” with APRI score >0.408, sensitivity and specificity were found to be 34% and 79%, respectively. In a study conducted by Korkmaz et al. with a large patient group (2520 patients, 40 centers), the sensitivity and specificity of the APRI score were calculated as 56.57% and 71.41%, respectively (21). Also, a correlation was found between the APRI scores of CHB patients and the presence of fibrosis in liver biopsy (22). In some studies, no correlation was found between the APRI and the presence of fibrosis in patients with CHB (23, 24).
When the FIB-4 scores of the patients were compared according to liver biopsy, there was no significant difference in the median scores (p=0.40 and p=0.77, respectively). When the patients were grouped according to liver biopsy fibrosis and evaluated by ROC analysis for FIB-4 score >0.70, which was obtained to differentiate patients with “no fibrosis and mild fibrosis” from patients with “severe fibrosis,” the sensitivity was 71%, and specificity was 46%; for FIB-4 >0.770, the sensitivity was 75%, and specificity was 47%. Studies on FIB-4 showed that liver biopsy could be avoided in patients with scores outside of 1.45-3.25 (25). In other studies, both sensitivity and specificity were 83% when the FIB-4 score was ≤1.45, and the sensitivity and specificity of FIB-4 score ≥3.25, showing significant fibrosis, were 47% and 80%, respectively (26).
The performance of a noninvasive diagnostic method for fibrosis in chronic liver disease was evaluated by comparing sensitivity, specificity, ROC curve, and area under the ROC curve (AUROC) data with liver biopsy. AUROC >0.90 is the ideal criterion for a good noninvasive biomarker (19, 20). In studies published in the literature, the observed AUROC values of the marker and biopsy fall in the range of 0.76-0.88. Although the AUC ratios in the ROC analyses performed in our study varied between 52% and 64%, it can be said that the sensitivity for FIB-4 and the specificity for APRI were better.
Since patients with cirrhosis are followed up by the gastroenterology clinic in our center, the number of patients with advanced fibrosis admitted to our clinic was small. In our study, low specificity values for APRI and FIB-4 scores were associated with a low number of severe fibrotic cases. Ho et al. found noninvasive scoring to be significantly superior in demonstrating liver fibrosis in patients diagnosed with chronic viral hepatitis C and developing hepatocellular carcinoma (26). In a study of 832 patients with HIV/HCV co-infection, the higher the liver fibrosis value of the patient group, the higher the reliability of noninvasive tests (25). Another study concluded that the higher the liver fibrosis value, the higher the reliability of noninvasive tests (27).
When the correlation between the calculated clinical scores of the patients was evaluated, there was a statistically significant linear relationship between the FIB-4 and APRI scores (r=0.51 and p<0.001). Other studies have shown that the APRI score alone is not sufficiently sensitive to exclude fibrosis, and its use in combination with other scores will provide higher diagnostic accuracy (28-30).
Our study has some limitations. The most important limitation is that the number of severe fibrosis cases at presentation was low because of the retrospective design of the study, and the liver histology of the patients could not be evaluated by the same pathologist.
In conclusion, noninvasive tests reduce the need for liver biopsy but do not eliminate it completely. Although studies on noninvasive methods have increased in recent years, a sufficient degree of accuracy has not been achieved. No noninvasive markers and threshold values have been clearly standardized because the methods developed cannot be applied in large patient populations, blood tests cannot be performed on the same day as the biopsy, the same fibrosis scoring system is not used in the evaluation, and the biopsy samples compared are not evaluated by pathologists with the same competence, different ethnic origins in the studies, and therefore different virus genotypes. The general recommendation is to use several noninvasive markers together or in combination with alternative noninvasive imaging methods, such as FibroScan.
Multicenter studies and meta-analyses in large groups of patients with chronic HBV will guide the determination of noninvasive markers that may be an alternative to invasive methods for determining disease activity in this patient group. We believe that our study will contribute to meta-analyses conducted on the evaluation of liver fibrosis using noninvasive methods in patients with hepatitis.