Introduction
In recent decades, fungal infections of the central nervous system (CNS) have increased significantly. Of more than 100,000 identified fungal species, approximately 10 to 15% are responsible for implicated fungal-related neurological diseases (1). A significant clinical manifestation of fungal infections of the CNS is meningitis, a serious condition marked by inflammation of the tissues surrounding the brain and spinal cord (2). Various fungi can cause this condition, including yeast species like Cryptococcus neoformans, Candida spp., Cryptococcus spp., and Trychosporon spp.; filamentous fungi such as Aspergillus spp., Penicillium spp., Pseudallescheria spp.; dimorphic fungi like Blastomyces dermatitidis, Histoplasma capsulatum, Coccidioides spp., and Sporothrix spp.; and dematiaceous fungi such as Cladophialophora bantiana and Exophiala dermatitidis (3).
Cryptococcus spp. is the leading cause of fungal meningitis worldwide, particularly affecting individuals with HIV. Recent studies indicate an annual mortality rate of approximately 180,000 AIDS patients due to cryptococcal meningitis, constituting 15% of all AIDS-related deaths (4, 5). C. neoformans is the primary cause of most cryptococcal meningitis cases among the Cryptococcus genus. Additionally, reports indicate numerous cases of Cryptococcus gattii in the Pacific Northwest and certain provinces of Canada (6, 7). Individuals in high-risk groups, such as AIDS patients, transplant recipients, those with weakened immune systems due to corticosteroid drugs and chemotherapy, and patients with hematologic malignancies, are most susceptible to neurological infections caused by pathogenic fungi. Moreover, non-sterile and unsanitary surgical instruments pose significant risks for meningitis in neurosurgery (3).
While Cryptococcus spp. is the most common cause of fungal meningitis, Candida spp. remains the most prevalent fungal pathogen in humans. Candida spp. often induces meningitis in premature infants, possibly due to the incompleteness of their blood-brain barrier, and in children with immune system defects. In contrast, Aspergillus spp. rarely causes CNS infections in premature infants but is known to cause meningitis in infants and children with hematological disorders or impaired immune systems (8).
The originality of this research is rooted in its worldwide perspective and emphasis on epidemiological data from various global regions. In contrast to numerous studies on fungal meningitis that often concentrate on particular countries or areas, this review synthesizes a broad array of epidemiological literature, thereby facilitating a thorough and comparative analysis of the disease’s prevalence, associated risk factors, and outcomes across different populations and healthcare systems. By investigating global trends and disparities, the study provides valuable insights into the geographic and demographic elements that affect the incidence and development of fungal meningitis, which can guide more focused public health initiatives and enhance the global healthcare response to this rising infectious challenge.
This article reviews the causative agents, demographic vulnerabilities, geographic variability, and diagnostic challenges of fungal meningitis, providing essential information for public health awareness. Diagnosing fungal meningitis presents numerous challenges, largely because its symptoms closely resemble those of meningitis caused by bacteria and viruses. Additional obstacles include the limitations of current diagnostic tests, which may involve the analysis of cerebrospinal fluid, the detection of fungal antigens, or the culture of fungi. These methods can be complex and time-consuming, often leading to delays in treatment. Such delays can increase the risks associated with the disease. Furthermore, in cases with a low fungal burden, traditional diagnostic methods and cultures exhibit low sensitivity, making detection difficult (9, 10).
Although emerging diagnostic techniques—such as advanced molecular diagnostics and cerebrospinal fluid β-D-glucan tests—show promise, they remain largely inaccessible, particularly in resource-limited settings (9, 11). Additionally, immunocompromised patients, including those with HIV/AIDS or those undergoing immunosuppressive therapy, are at a higher risk for delayed diagnosis due to the atypical presentations of their infections (4).
The prognosis of fungal meningitis is influenced by several factors, including the causative agent, the patient’s immune status, and the timing of diagnosis and treatment. For instance, when cryptococcus is the causative agent, which typically affects immunocompromised individuals, delays in initiating treatment can significantly increase morbidity and mortality rates (12). Early diagnosis and appropriate treatment generally lead to improved outcomes; however, studies indicate that neurological complications may persist even after early intervention. Despite advancements in treatment options, mortality rates continue to rise among these patients. Emerging therapies and enhanced diagnostic methods, such as molecular diagnostics, aim to improve these outcomes (13). The findings presented in this review can guide future research by identifying gaps in understanding disease-causing factors and vulnerable populations.
Materials and Methods
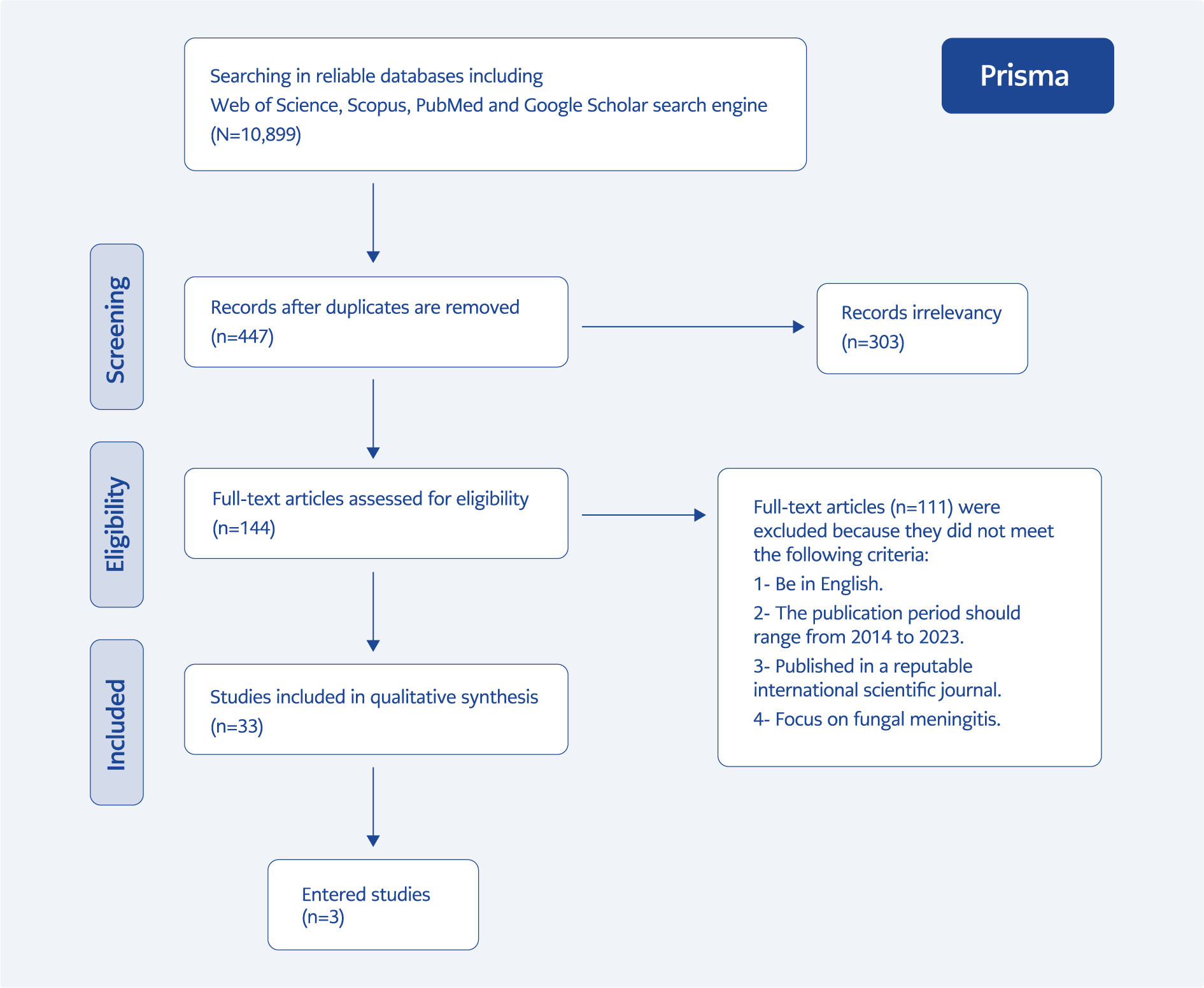
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (14). It is a systematic review of fungal meningitis that examines a collection of English articles.
We searched the databases Web of Science, Scopus, PubMed, and Google Scholar using the following English keywords: “meningitis and CNS fungal infections,” “fungal meningitis,” “fungal meningitides,” “Blastomyces,” “Histoplasma,” “Aspergillus,” “Penicillium,” “Sporothrix,” “Pseudallescheria,” “Candida,” and “Coccidioides.”. Based on Medical Subjects Headings (MeSH) terms, the search period covered January 2014 through January 2023. We also performed combination searches using Boolean operators (AND, OR) to enhance the search strategy. Two authors manually reviewed the titles generated from the initial search to ensure all relevant sources were included.
In the next step, abstracts of all retrieved articles were reviewed, and studies unrelated to the topic were excluded based on predefined eligibility criteria (1): 1) articles must be written in English, 2) published between 2014 and 2023, 3) published in reputable scientific journals, 4) focused on fungal meningitis. Reasons for exclusion were documented to prevent bias and errors. Full texts of selected articles were retrieved, and studies without accessible full texts were excluded.
The full texts of the retained articles were reviewed and categorized by title, first author’s name, year of publication, data collection methods, and key findings. The quality of each study was assessed using the Joanna Briggs Institute (JBI) tools. The findings were synthesized using the PRISMA framework to ensure a systematic, comprehensive, and unbiased review of the literature on fungal meningitis.
Results
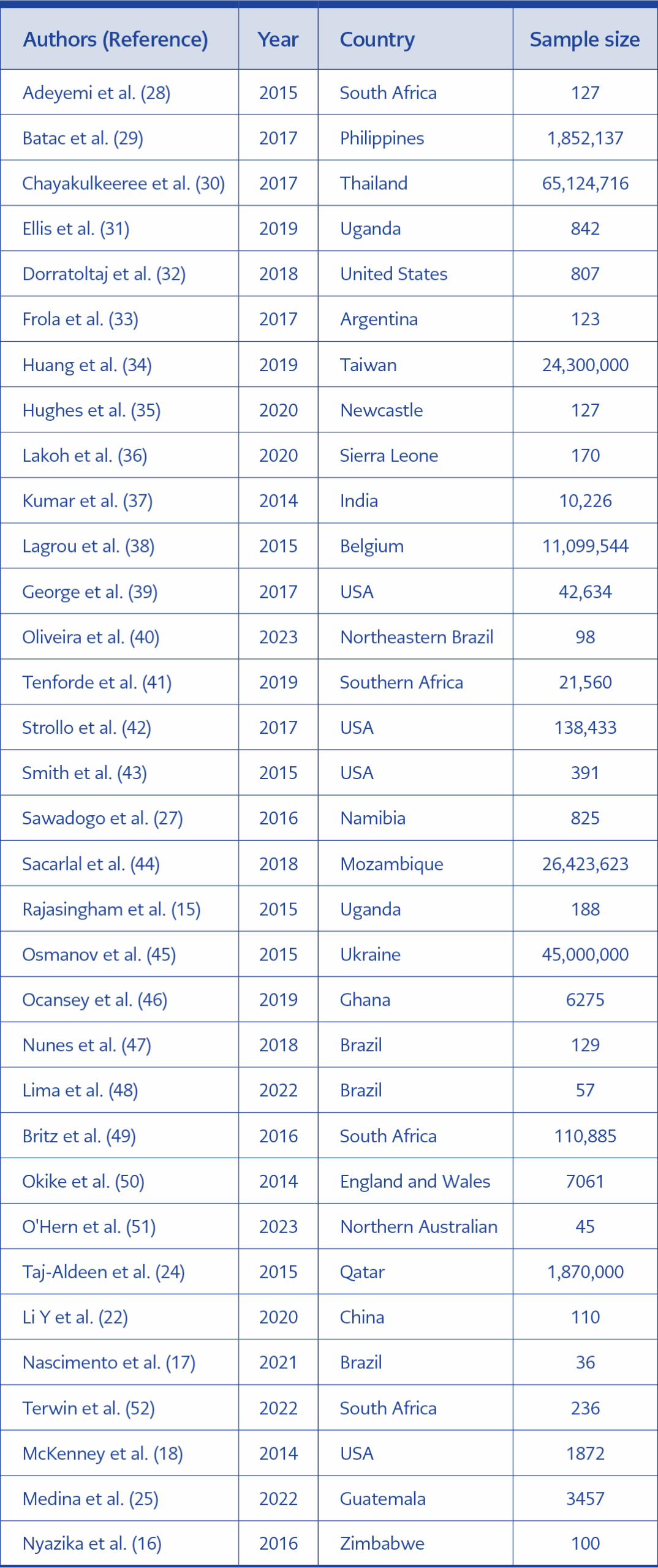
Following a systematic search of databases and other sources, 33 studies were retrieved and screened for eligibility. Figure 1 presents a summary of the study’s PRISMA flowchart. All 33 studies were included in this descriptive review and used for the qualitative/narrative synthesis. The risk of bias was assessed using the Newcastle-Ottawa Scale (NOS) tool, with all studies scored between 6 and 9, indicating at least a moderate level of quality. The characteristics of the included studies are summarized in Table 1.
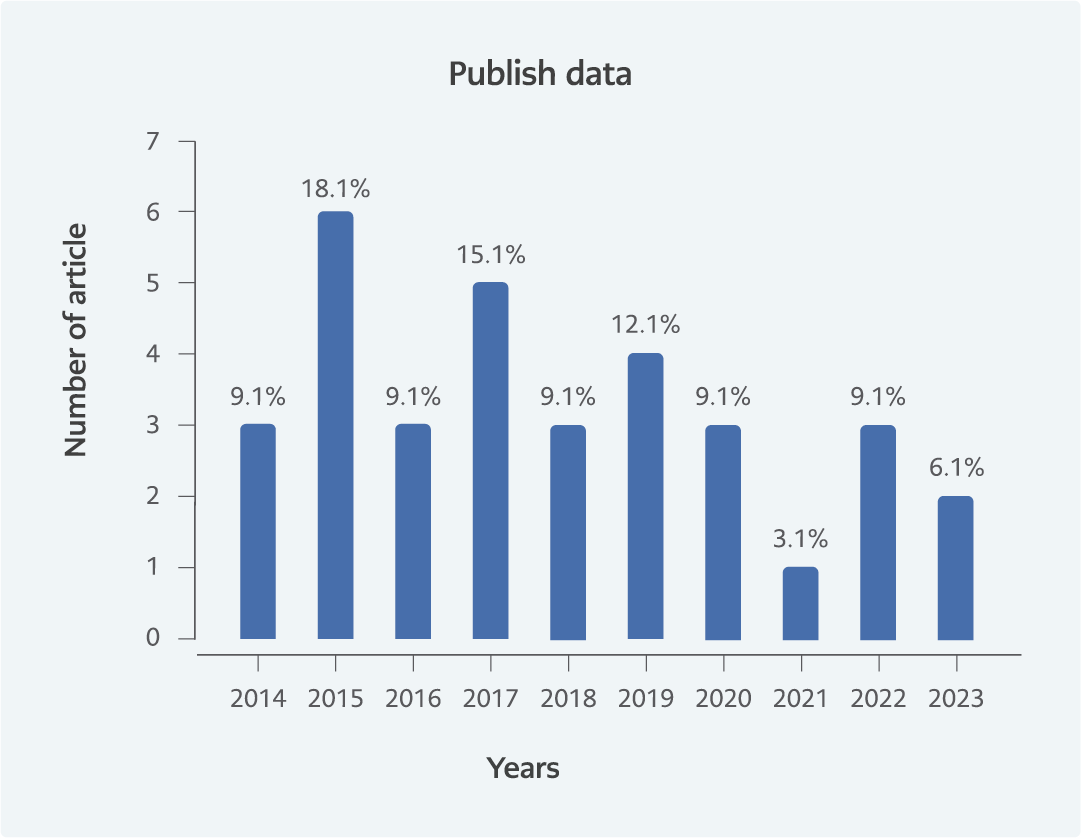
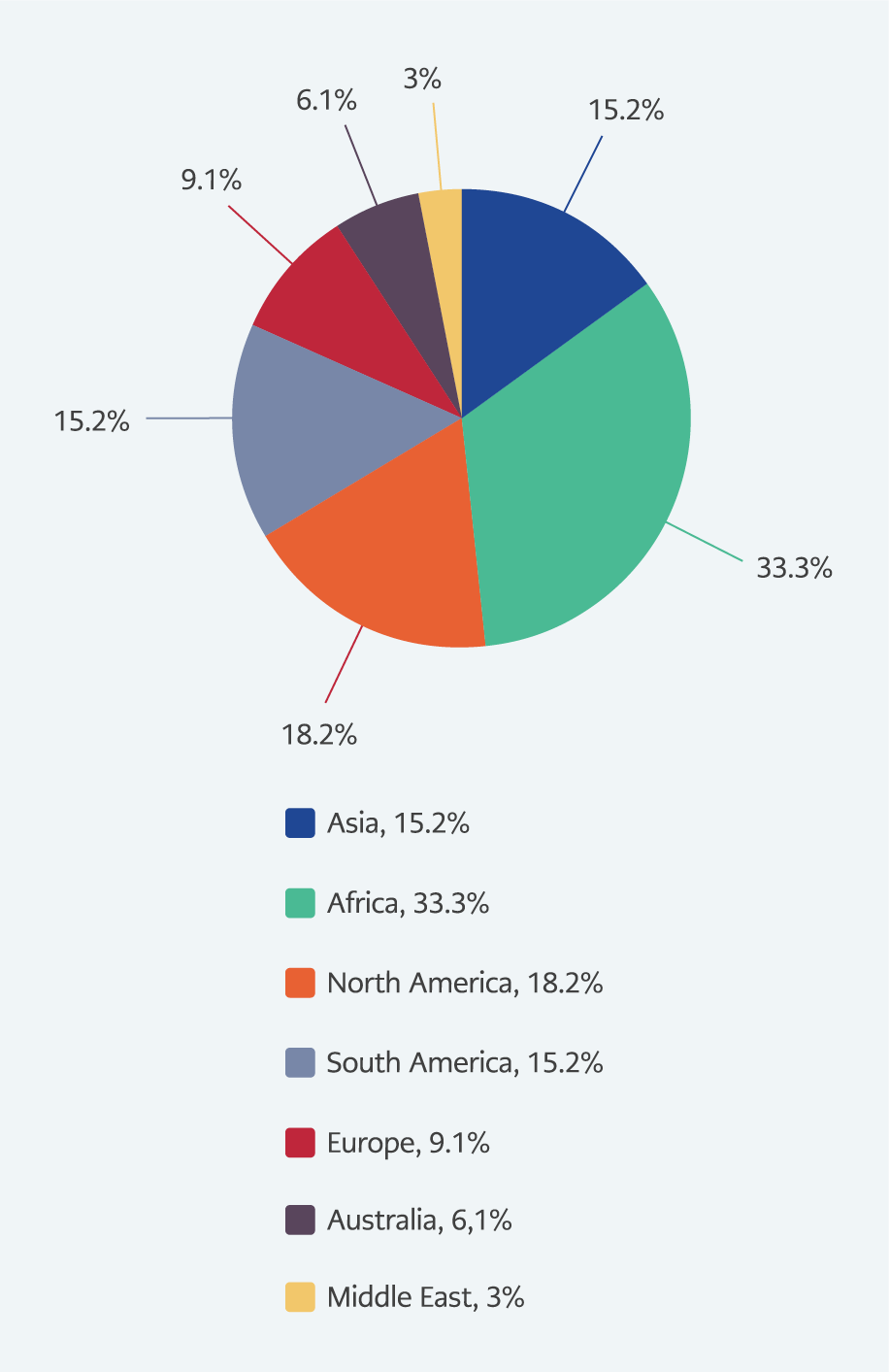
Most studies (60.5%) were published before 2018 (Figure 2). Among them, 16 studies focused on the general population, eight on hospitalized individuals, and nine on individuals diagnosed with AIDS. Sample sizes ranged widely, from 36 to 65,124,716 participants. The majority of the studies were conducted in the United States (5), Southern African countries (4), and Brazil (3) (Figures 3).
Gender data was reported in 42% of the studies. Among these, the majority of participants were male, with male representation ranging from 88% to 12% and female representation ranging from 12% to 87% —less than 1% of participants identified as transgender. In terms of age, 12% of the research specifically targeted individuals over the age of 18, while 42% included participants from all age groups.
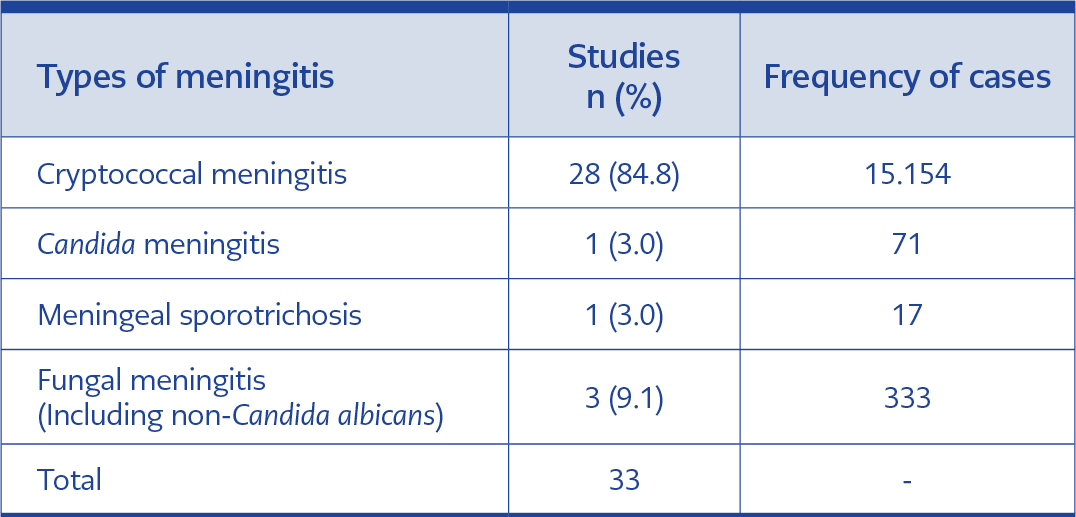
The majority of studies (84.8%) documented cases of cryptococcal meningitis. In contrast, only one study reported cases of sporotrichosis meningitis, with a 100% prevalence among those with sporotrichosis. Candida meningitis was mentioned in 3% of the studies, with a prevalence of 18% among patients. Additionally, 27% of the studies reported fungal meningitis without specifying the species or genus of the causative agent (Table 2).
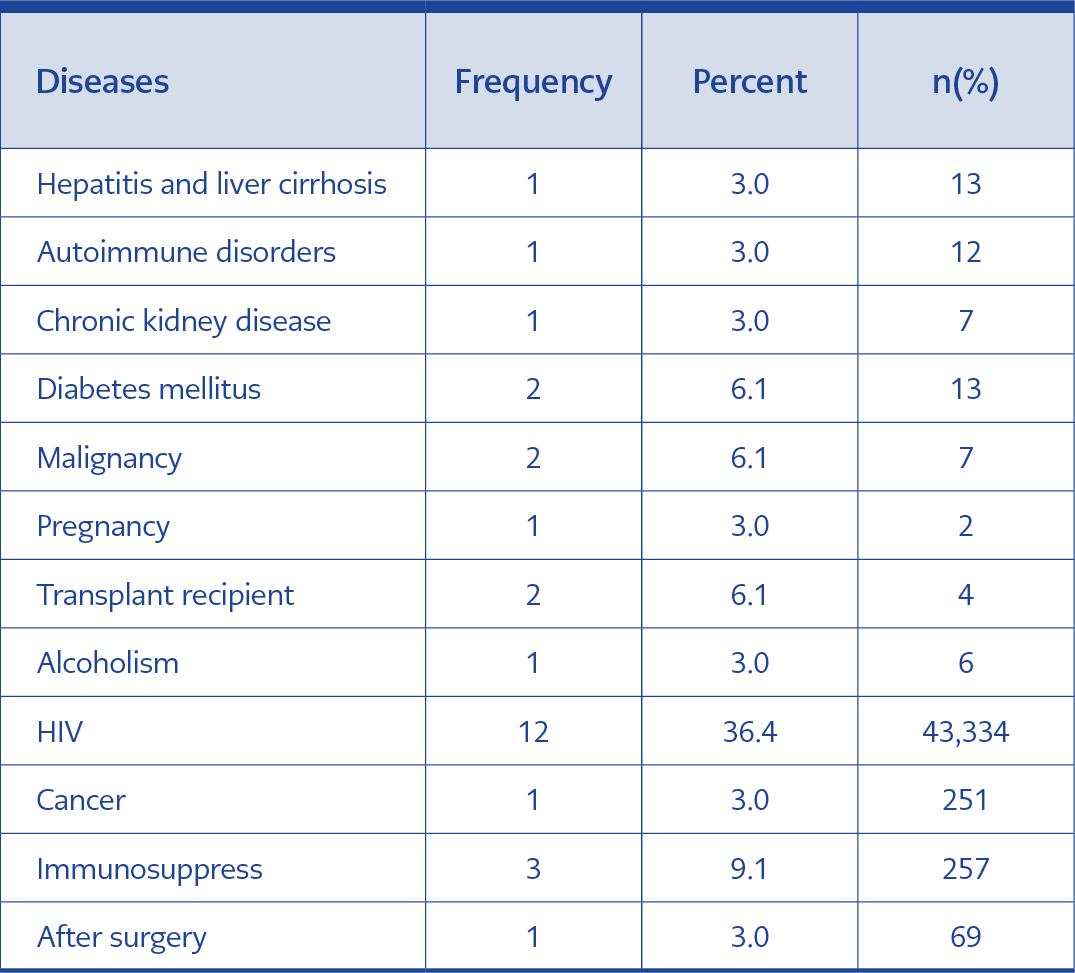
In 15% of the studies, C. neoformans was directly identified as the causative agent of meningitis, with prevalence among patients ranging from 56% to 100%. Overall, Cryptococcus spp. was reported as the cause of meningitis in 85% of the included studies. In 28 out of 33 studies, various physiological and pathological conditions were documented, with the most common being HIV (36.4%), immunosuppressed (9.1%), and organ transplantation (6%) (Table 3).
A total of 33% of the studies focused on individuals with AIDS, among whom fungal meningitis prevalence ranged from 4.5% to 100%. The association between meningitis and cancer was reported in 6% of the studies, with cancer patients representing less than 25% of all meningitis cases. Immunodeficiency was discussed in 9% of the studies, with the rate of affected patients ranging from 2% to 81%. Additionally, one study highlighted fungal meningitis as a postoperative complication.
Discussion
This systematic review presents an overview of the global epidemiology and clinical characteristics of fungal meningitis, with a specific focus on cryptococcal meningitis. The findings highlight the significant burden of this disease, especially among immunocompromised individuals, such as those living with HIV/AIDS.
The majority of included studies (84.8%) reported cases of cryptococcal meningitis, which aligns with previous literature identifying Cryptococcus species as the leading cause of fungal meningitis worldwide (15). Cryptococcal meningitis was predominantly attributed to C. neoformans sensu stricto, consistent with reports indicating that C. neoformans is responsible for most HIV-associated cryptococcosis cases in sub-Saharan Africa (16). However, the study by Nascimento et al. (17) also found cases caused by the C. gattii species complex in non-HIV patients in Brazil, underscoring the importance of considering both species complexes.
The high prevalence of cryptococcal meningitis among HIV/AIDS patients (36.4%) is a concerning finding, corroborating the global burden estimates by Rajasingham et al. (4), emphasizing the need for improved prevention, early detection, and effective management strategies in this high-risk population. For example, McKenney et al. (18) reported a lower cryptococcal antigen (CrAg) positivity rate of 2.9% among HIV patients in the United States, potentially reflecting differences in access to antiretroviral therapy (ART) and healthcare resources. To address these challenges, implementing routine CrAg screening in HIV-positive individuals with low CD4 counts can facilitate early detection and preemptive antifungal therapy, thereby reducing the progression to meningitis and associated mortality (19). Enhancing access to ART and ensuring adherence is crucial for restoring immune function and mitigating the incidence of opportunistic infections like cryptococcal meningitis (20). Additionally, education and awareness programs for both healthcare providers and patients can promote timely recognition and intervention, further improving patient outcomes (21).
Interestingly, a significant proportion of cases (9.1% immunosuppressed, 6.1% malignancy, 6.1% transplant recipients) occurred in non-HIV immunocompromised individuals, underscoring the importance of considering fungal meningitis in these vulnerable populations as well. Li et al. (22) found that 40% of cryptococcal meningitis cases in China occurred in individuals without underlying conditions, suggesting that immunocompetent individuals may also be at risk. For these populations, prophylactic antifungal therapies and stringent infection control practices in healthcare settings are essential to prevent nosocomial transmission and manage existing vulnerabilities (23).
The geographical distribution of studies included in this review indicates a concentration of research in certain regions, such as the Americas, southern Africa, and Brazil. However, the study by Taj-Aldeen et al. (24) provides valuable insights into the burden of fungal infections in Qatar, highlighting the need for more regional data to inform public health policies and resource allocation.
While cryptococcal meningitis was the predominant focus, other forms of fungal meningitis, such as candidiasis and sporotrichosis, were also reported, albeit at lower frequencies. This diversity of causative agents underscores the importance of accurate diagnosis and tailored treatment approaches. The reported mortality rates for cryptococcal meningitis varied across studies, ranging from 30.8% in Guatemala (25) to 55.6% in Zimbabwe (16). These high mortality rates, particularly in resource-limited settings, emphasize the urgent need for improved access to diagnostic tools, antifungal therapies, and comprehensive care for affected individuals. The deployment of rapid diagnostic tests, such as lateral flow assays for CrAg, can facilitate early diagnosis and prompt initiation of treatment, thereby reducing mortality rates (26).
Several studies identified factors associated with poor outcomes, such as treatment delays, interruptions in induction therapy, and the presence of comorbidities like end-stage kidney disease (27). Additionally, the occurrence of immune reconstitution inflammatory syndrome (IRIS) in some cases (27) highlights the complexities of managing fungal meningitis in the context of immune system recovery.
The findings from this systematic review underscore the substantial global burden of fungal meningitis, particularly cryptococcal meningitis, among HIV/AIDS patients and other immunocompromised populations. Despite advances in understanding the epidemiology and clinical features of these infections, significant challenges remain in early diagnosis, treatment access, and management of complications. Continued research, enhanced surveillance, and improved access to healthcare resources are essential to mitigating the impact of this potentially life-threatening condition worldwide.
This review has several limitations. The exclusion of non-English studies may have omitted relevant research from non-English-speaking regions, potentially introducing language bias. Additionally, the variability in study designs and quality may affect the comparability of results. Publication bias is another concern, as studies with significant findings are more likely to be published. Furthermore, the heterogeneity among included studies in terms of population demographics, diagnostic criteria, and treatment protocols limits the ability to generalize the findings universally.
Future research should focus on expanding epidemiological studies to underrepresented regions, standardizing diagnostic criteria, and exploring the impact of emerging antifungal therapies. Enhanced surveillance and data sharing can facilitate a more accurate global understanding of fungal meningitis trends and inform targeted public health strategies. Additionally, research into developing novel antifungal agents and vaccines could provide long-term solutions for preventing fungal meningitis in high-risk populations.
Conclusion
Fungal meningitis, particularly cryptococcal meningitis, poses a substantial global health burden, especially among immunocompromised individuals. Addressing the challenges of early diagnosis, treatment accessibility, and comprehensive care is essential for reducing mortality and improving outcomes. Implementing targeted prevention strategies, such as routine antigen screening and prophylactic therapies, alongside standardized treatment protocols, can significantly mitigate the impact of this life-threatening condition. Continued research and international collaboration are vital to enhancing prevention, control, and management efforts worldwide.