Introduction
The coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), led to significant hospitalizations and mortality globally from 2019 to 2021. According to data from the World Health Organization (WHO), over 776 million COVID-19 cases and more than 7 million COVID-19-related deaths have been reported to date (1). Although the disease’s significance has diminished due to widespread vaccination, isolation protocols, and the growth of herd immunity, the persistent risk of a pandemic arising from novel mutations sustains its importance in public health discourse.
Since the beginning of the pandemic, laboratory markers have played a critical role in evaluating COVID-19 prognosis. Numerous laboratory markers have been identified in the literature for assessing prognosis following the onset of the disease (2-4). Studies on COVID-19-associated prognostic laboratory markers often focus on measurements taken on the first day of hospitalization or intensive care unit (ICU) admission (5-7). A single time-point measurement may not provide sufficient information on how prognostic predictors change over time (8). Serial monitoring of specific biochemical parameters has been demonstrated to provide additional information in comparison with a single measurement taken at the time of admission. Serial monitoring of routine tests has been shown to be important for predicting patient prognosis (9). There are limited studies in the literature on the role of serial monitoring of laboratory parameters in predicting the need for intensive care and mortality.
The primary aim of this study was to analyze the temporal monitoring patterns of serum biomarkers associated with the necessity for intensive care in severe COVID-19 cases and to elucidate their prognostic significance in predicting unfavorable clinical outcomes.
Materials and Methods
Study Design and Sample
This study was designed as a single-center, observational, retrospective study conducted at a training and research hospital. All patients aged 18 years and older who were diagnosed with severe COVID-19 by polymerase chain reaction (PCR) testing and followed up with hospitalization between March 1, 2021, and November 30, 2021, were included. Patients were excluded if they were under 18 years of age, had inaccessible medical records, lacked laboratory parameter monitoring, were pregnant, and were diagnosed with COVID-19 by thoracic tomography but had negative PCR test results.
Study Protocol
The patients were categorized into two cohorts: those necessitating intensive care and those who did not. Serial laboratory evaluations were performed from the point of ward admission until the transition to intensive care. Measurements taken after ICU admission were excluded from the study. Due to our study’s observational and retrospective nature, we based our analysis on the routine laboratory follow-up trends of clinicians. As clinicians’ follow-up routine was every other day, serial laboratory measurements — including lymphocyte count, platelet (PLT) count, C-reactive protein (CRP), aspartate aminotransferase (AST), alanine aminotransferase (ALT), D-dimer, ferritin, lactate dehydrogenase (LDH), and troponin I — were recorded on days 0, 2, 4, 6, and 8 from hospitalization to ICU admission.
Severe COVID-19 pneumonia was defined by clinical symptoms such as fever, cough, dyspnea, tachypnoea, and respiratory rate > 30/minute, SpO2 < 90% in room air (10). The need for intensive care was assessed in accordance with the Turkish Ministry of Health’s guidelines for the management of the novel coronavirus (COVID-19) (11). Patients requiring intensive care were compared with those who did not in terms of demographic characteristics, clinical features, and serial laboratory measurements. The patients included in our study were followed up in the ward with a diagnosis of severe COVID-19, and corticosteroid treatment was administered to all patients as they required oxygen therapy according to the definition of severe COVID-19.
Demographic information, clinical data, and laboratory results of the patients included in the study were obtained from the hospital database, the e-Nabız Personal Health System, and the Public Health Management System of the Turkish Ministry of Health. The study was approved by the Ethics Committee of Yıldırım Beyazıt University Yenimahalle Training and Research Hospital on November 5, 2022, with decision number E-2021-73.
Statistical Analysis
Statistical analyses were conducted using IBM SPSS Statistics for Windows, version 23.0 (IBM Corp., Armonk, NY, USA), and GraphPad Prism, version 8.0 (GraphPad Software, San Diego, CA, USA) was used for graphical illustrations. Statistical significance was set as p<0.05. Descriptive statistics for continuous variables were presented as the median and interquartile range (IQR 25th–75th percentiles), while categorical data were presented as frequencies and percentages. The Kolmogorov-Smirnov test and histograms were used to assess the normality of data distribution. Chi-square and Fisher’s exact tests were applied to compare nominal variables across groups. The independent samples t-test was used to compare normally distributed data, while the Mann-Whitney U test was used for non-normally distributed data.
In order to assess the predictive value of laboratory parameters for the development of intensive care needs in COVID-19 patients, the receiver-operating characteristic (ROC) curves were constructed for each measurement day, and the area under the curve (AUC) was calculated. AUC values greater than 0.70 were considered diagnostically significant for predicting intensive care requirements, and the day with the highest AUC was identified. The threshold values at which the AUC is considered significant vary across different sources. Generally, in the literature, AUC values between 0.7 and 0.8 are deemed acceptable, 0.8 to 0.9 are considered excellent, and values above 0.9 are regarded as outstanding. Accordingly, in our study, an AUC of 0.7 or higher was evaluated as significant (12,13). Sensitivity and specificity were calculated for the cut-off points with the optimal values. The cut-off values were calculated using the Youden Index.
Results
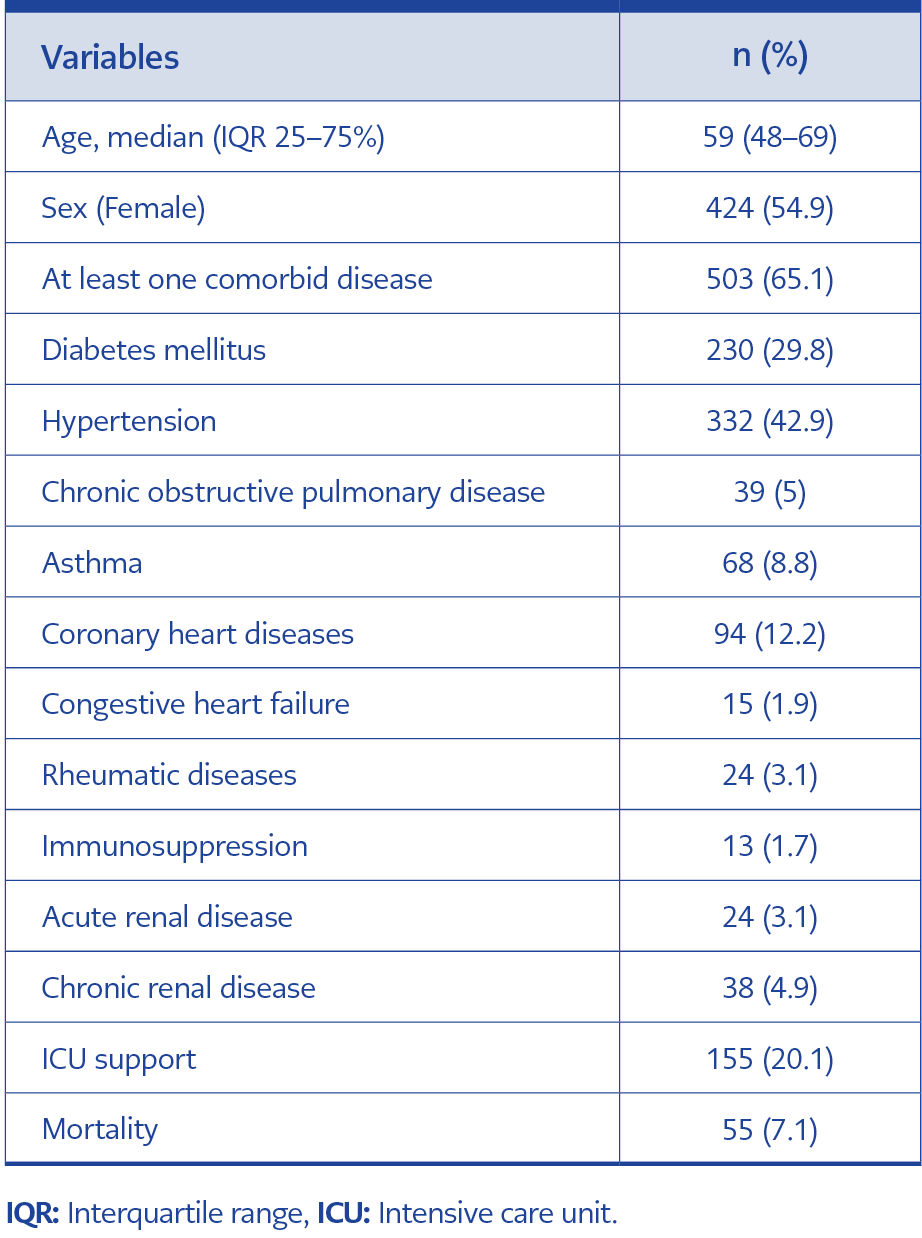
A total of 773 patients were included. The median age was 59 (IQR 48–69), 54.9% were female, and 65.1% had at least one comorbid disease. Intensive care was required in 20.1% of the patient cohort. The demographic and clinical characteristics of the patients are presented in Table 1.
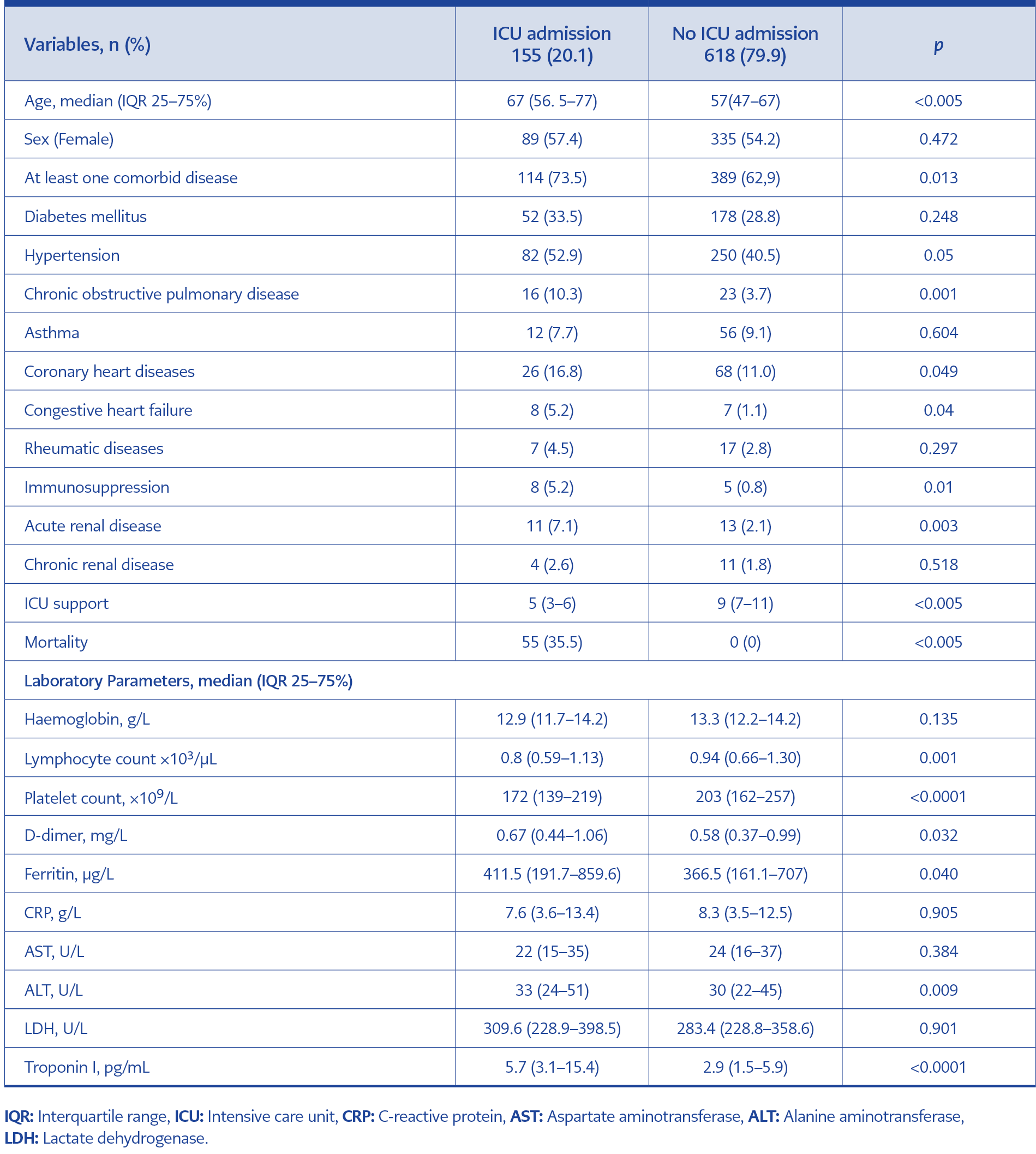
The demographic, clinical data, and laboratory values on the first day of hospitalization of patients requiring and not requiring intensive care were compared statistically. Patients requiring intensive care were found to be older and have more comorbidities than those who did not. The data are presented in Table 2.
Serial laboratory values measured on days 0, 2, 4, 6, and 8 of hospital stay were compared between the groups. As patients requiring intensive care were excluded from further analysis after ICU admission, data from 773 patients on day 0, 744 on day 2, 689 on day 4, 544 on day 6, and 359 on day 8 were included in the evaluation.
In the cohort not requiring intensive care, lymphocyte counts exhibited a progressive upward trend, whereas CRP levels showed a steady decline. Platelet counts increased consistently across both groups, while troponin I levels remained stable. Conversely, other laboratory parameters displayed notable variability.
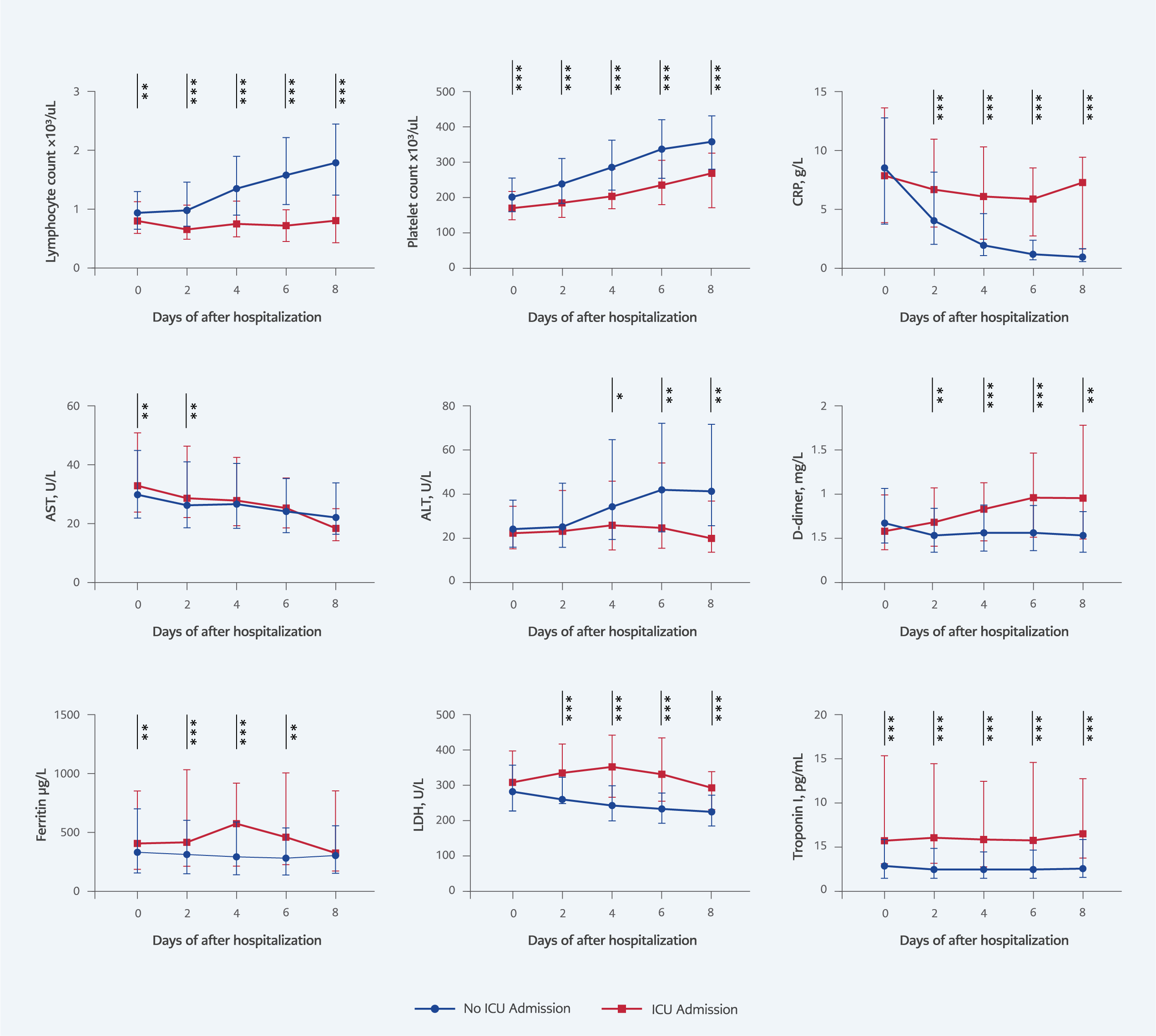
Figure 1. Comparison of serial laboratory measurements between groups with and without the need for intensive care.
ICU: Intensive Care Unit, CRP: C-reactive protein, AST: Aspartate aminotransferase, ALT: Alanine aminotransferase, LDH: Lactate dehydrogenase. *p<0.05, **p<0.01, ***p<0.001.
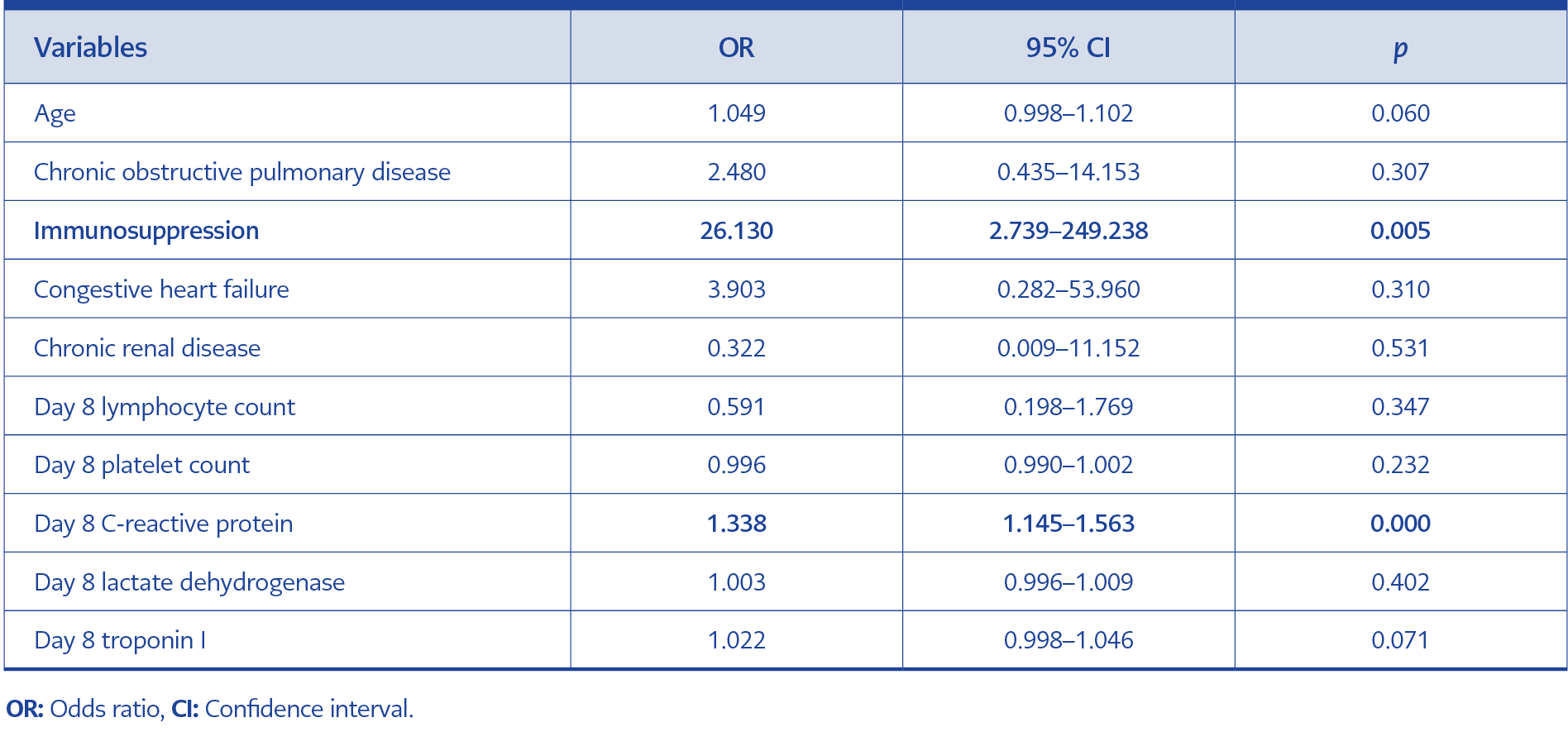
In the statistical comparison, lymphocyte count, PLT, and troponin I were found to be significantly different between the two groups in all measurements. CRP, D-dimer, and LDH showed significant differences between the groups on days 2, 4, 6, and 8. Figure 1 presents the comparisons and statistical analyses between the groups. We performed a multivariate analysis, including a model integrating parameters predicting progression to intensive care. The results of the multivariate analysis are presented in Table 3. The analysis showed that CRP level on day 8 and immunosuppression were independent risk factors.
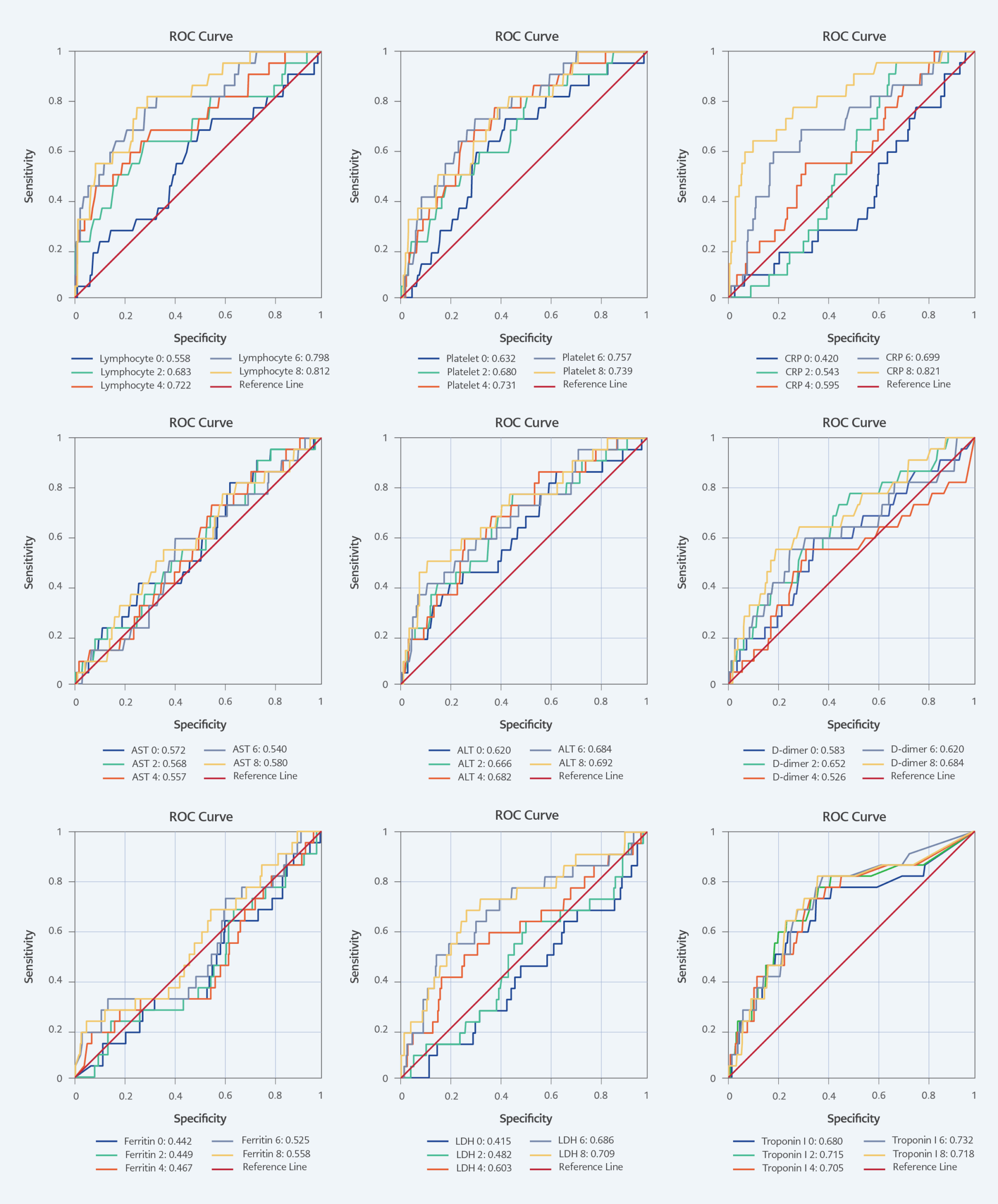
Figure 2. ROC curves and AUC values for each serial laboratory measurement.
AUC: Area under the curve, CRP: C-reactive protein, AST: Aspartate aminotransferase, ALT: Alanine aminotransferase.
ROC curves and AUC values for each serial laboratory measurement in predicting the development of intensive care needs in COVID-19 are presented in Figure 2. The AUC values of lymphocyte count, PLT, CRP, LDH, and troponin I measurements increased in a time-dependent manner from day 0 to day 8, with an observed increase in statistical significance.
Lymphocyte count on day 8 (AUC 0.812; cut-off value, 475), PLT on day 6 (AUC 0.757; cut-off value, 119,000), CRP on day 8 (AUC 0.821; cut-off value, 12.2), LDH on day 8 (AUC 0.709; cut-off value, 591.8), and troponin I on day 6 (AUC 0.732; cut-off value, 50.5) were found to be the most significant in predicting intensive care needs. ALT, AST, ferritin, and D-dimer measurements did not show statistical significance.
Discussion
Our study’s findings indicate that the serial monitoring of lymphocyte count, PLT, CRP, LDH, and troponin I measurements are significantly predictive in determining the need for intensive care in COVID-19 patients, and the diagnostic value of these parameters increases over time as patient follow-up days progress.
Lymphopenia is one of the key laboratory markers associated with poor outcomes in COVID-19 (14,15). In our study, while the lymphocyte count remained stable in patients requiring intensive care, it tended to increase over time in those who did not. ROC analyses revealed that lymphocyte count became more predictive of the need for intensive care as follow-up days increased. Similarly, a single-center study from China at the onset of the pandemic demonstrated that lymphocyte counts were significantly lower in the fatal group throughout the disease course (15). Chen et al. (16) also reported an increasing trend in lymphocyte counts among survivors, while in the group without mortality, lymphocytes remained low without a significant increase. Another single-center study yielded similar findings (17).
Although dynamic changes in lymphocyte counts were generally associated with mortality and the need for intensive care, some studies have presented conflicting results. In one single-center cohort study, the dynamic change in lymphocyte count was not found to be associated with mortality (9), while another study noted that although lymphocyte counts differed significantly between poor and good outcome groups, no stable trend was observed during dynamic follow-up (18). Tuncer et al. (19) reported that National Early Warning Score
(NEWS2), procalcitonin, neutrophil-to-lymphocyteratio (NLR), and albumin were predictive parameters for ICU admission and mortality on days 3, 5, and 7 of hospitalization. In addition, a strong correlation was found between NEWS2 and laboratory parameters, including lymphocyte count, neutrophil count, NLR, platelet-to-lymphocyte ratio (PLR), CRP, procalcitonin, ferritin, and urea on days 0, 3, 5 and 7. Our findings suggest that patients whose lymphocyte counts do not increase during follow-up should be closely monitored for potential intensive care needs.
Corticosteroids have been demonstrated to increase hemoglobin levels in the blood by delaying erythrophagocytosis (20). Furthermore, the treatment has been shown to cause neutrophilia and lymphopenia by increasing the number of neutrophils in peripheral blood (21). However, it should be noted that all patients received corticosteroid treatment. In the multivariate analysis (Table 3), no significant difference was found in lymphocyte count in serial measurements.
Platelet count, another hematological follow-up parameter, showed a significant reduction in the group requiring intensive care, similar to lymphocyte count, and its diagnostic value also tended to increase with longer follow-up. Siavoshi et al. (18) found that a daily average increase of 5.2% in PLT was associated with a better prognosis. Another study associated low and stable platelet counts with increased mortality, in contrast to higher and/or rising platelet counts (22).
CRP has been recognized as a critical biomarker in severe COVID-19 cases, indicating disease progression (23). In our study, CRP levels demonstrated a significant decline over time in patients who did not require intensive care, and its diagnostic accuracy in predicting intensive care needs was markedly improved in the ROC analysis. This finding is consistent with the general literature (17,18). Due to the design of our study, we excluded patients who progressed to intensive care, preventing us from obtaining follow-up values in those cases. Therefore, we believe our results highlight the significance of CRP in predicting intensive care needs, excluding factors such as secondary bacterial infections or treatments like interleukin-6 (IL-6) inhibitors, which could suppress CRP response.
Another biomarker whose diagnostic value increased over time was LDH. A modeling study evaluating 14 biomarkers in severe and critical COVID-19 patients found that decreasing LDH levels in serial follow-ups were the most significant predictor of hospital stay and survival (22). Li et al. (24) also identified LDH as possessing the highest independent sensitivity in determining prognosis. Similarly, another single-center study reported that a daily 2.5% reduction in LDH levels was associated with recovery (18).
SARS-CoV-2 infection is associated with cardiac damage and myocarditis. Consequently, dynamic monitoring of cardiac biomarkers has been found to be valuable in detecting potential cardiac injury and forecasting adverse outcomes (25). In our study, troponin I levels remained stable in both groups; however, its diagnostic value for predicting the need for intensive care increased over time. Therefore, we consider troponin I a crucial biomarker in assessing the requirement for intensive care in severe COVID-19 cases.
Our study has several limitations. First, as a single-center retrospective study, its findings may not be broadly applicable. Second, we did not assess the relationship between dynamic changes in laboratory parameters and patient clinical outcomes. Lastly, due to limited access, we were unable to evaluate serial follow-up results for viral load, which is known to be linked with poor prognosis (26,27). Despite these limitations, our study contributes valuable insights into the prognostic significance of dynamic laboratory monitoring in COVID-19.
The findings of our study suggest that consistent follow-up of lymphocyte and platelet counts, CRP, LDH, and troponin I can provide clinicians with vital information regarding the progression of the disease and the likelihood of intensive care requirements. Early identification of patients at higher risk for severe outcomes could enhance clinical decision-making and resource allocation, particularly in overwhelmed healthcare settings during a pandemic. Future research should validate these findings in larger, multicenter cohorts and incorporate additional factors, such as viral load and clinical correlates, to better understand the interplay between laboratory markers and disease severity in COVID-19. Furthermore, understanding the impact of different therapeutic interventions on these biomarkers and their ability to predict patient outcomes will be crucial in optimizing treatment strategies for COVID-19 and other similar infectious diseases.