Introduction
Antibiotic resistance has become a significant public health concern, primarily due to irrational antibiotic use (1). Healthcare and antimicrobial stewardship depend on using antibiotics correctly for several reasons. In the first place, adhering to the prescribed dosage ensures that the body receives the right amount of antibiotics to treat infections effectively. Second, appropriate dosing minimizes the likelihood of adverse effects associated with antibiotic use, improving patient safety. Third, consistent administration of the correct dosage contributes to establishing predictable pharmacokinetic profiles, making accurate dosing adjustments possible for patients with special needs, such as pediatrics or geriatrics, as well as renal or hepatic impairments (2-4). Additionally, adhering to the correct dosage regimen contributes to efforts to combat antimicrobial resistance and preserve antibiotic efficacy for future generations.
Augmented renal clearance (ARC) was first defined as increased excretion of solutes relative to baseline, a process involving glomerular filtration and tubular function changes (5). In a clinical setting, ARC refers to a creatinine clearance (CrCl) exceeding 130 mL/min/1.73m² (6, 7).
Although no precise mechanism exists for ARC (8, 9), three main mechanisms have been advocated by an analysis of the literature (9). The first is hyperkinetic events that can occur in conditions such as sepsis, burns, major surgery, and severe trauma, regardless of whether or not there is an infection (10, 11). The second involves renal function reserve, in which the kidney’s capacity to increase glomerular filtration rate (GFR) under certain circumstances, including hyperfiltration states, cardiorenal conditions, etc. (12). The third is the concept described as “brain-kidney crosstalk,” which has recently been linked to ARC (13).
ARC can significantly impact the pharmacokinetics of various antimicrobials, particularly those eliminated primarily via renal excretion. Antibiotics such as β-lactams (e.g., carbapenems, cephalosporins, and penicillins), glycopeptides (e.g., vancomycin), aminoglycosides, and oxazolidinones (e.g., linezolid) are among the most affected. Increased renal clearance associated with ARC may lead to subtherapeutic drug concentrations, potentially compromising clinical efficacy, particularly in critically ill patients. This underscores the importance of understanding how ARC influences specific antimicrobials to optimize dosing strategies and maintain therapeutic outcomes (14-18).
Due to variability in the quality and completeness of data across studies, synthesizing the data was challenging. Therefore, we selected the scoping review method. Although there are reviews (19, 20) and original studies in the literature that have investigated the impact of ARC on antibiotics, such as β-lactam (21) and vancomycin (22), no scoping review to date evaluated all antimicrobials in the adult population (18). The present review is the first scoping review focusing on the influence of ARC on antimicrobial therapy in adult patients. This review aimed to summarize the current evidence regarding ARC in adult patients receiving antimicrobials over the past five years, focusing on its prevalence, risk factors, and impact on achieving therapeutic drug levels.
Materials and Methods
The PRISMA-ScR guideline was followed in this scoping review (23). No review protocol was established for the current study.
Search Strategy
The search was conducted on December 19, 2023, using three scientific databases: Web of Science, PubMed, and Scopus. The keywords used in the search were “enhanced renal function “OR” augmented renal function “OR” augmented renal clearance “OR” enhanced renal clearance”, which were applied to the title, abstract, or keywords fields; and antibiot* OR antimicr* OR antibact* in all search fields of the studies. The findings were limited to the last five years, between 2019 and 2023.
Research Questions
In the current study, the following questions were addressed:
1. What are the main characteristics of ARC studies in adult patients receiving antimicrobials?
2. What is the definition, prevalence, and risk factors of ARC in adult patients receiving antimicrobials?
3. Are there recommended approaches to minimize the effect of ARC on antimicrobial levels in adults?
4. What are the gaps for future research?
Article Selection
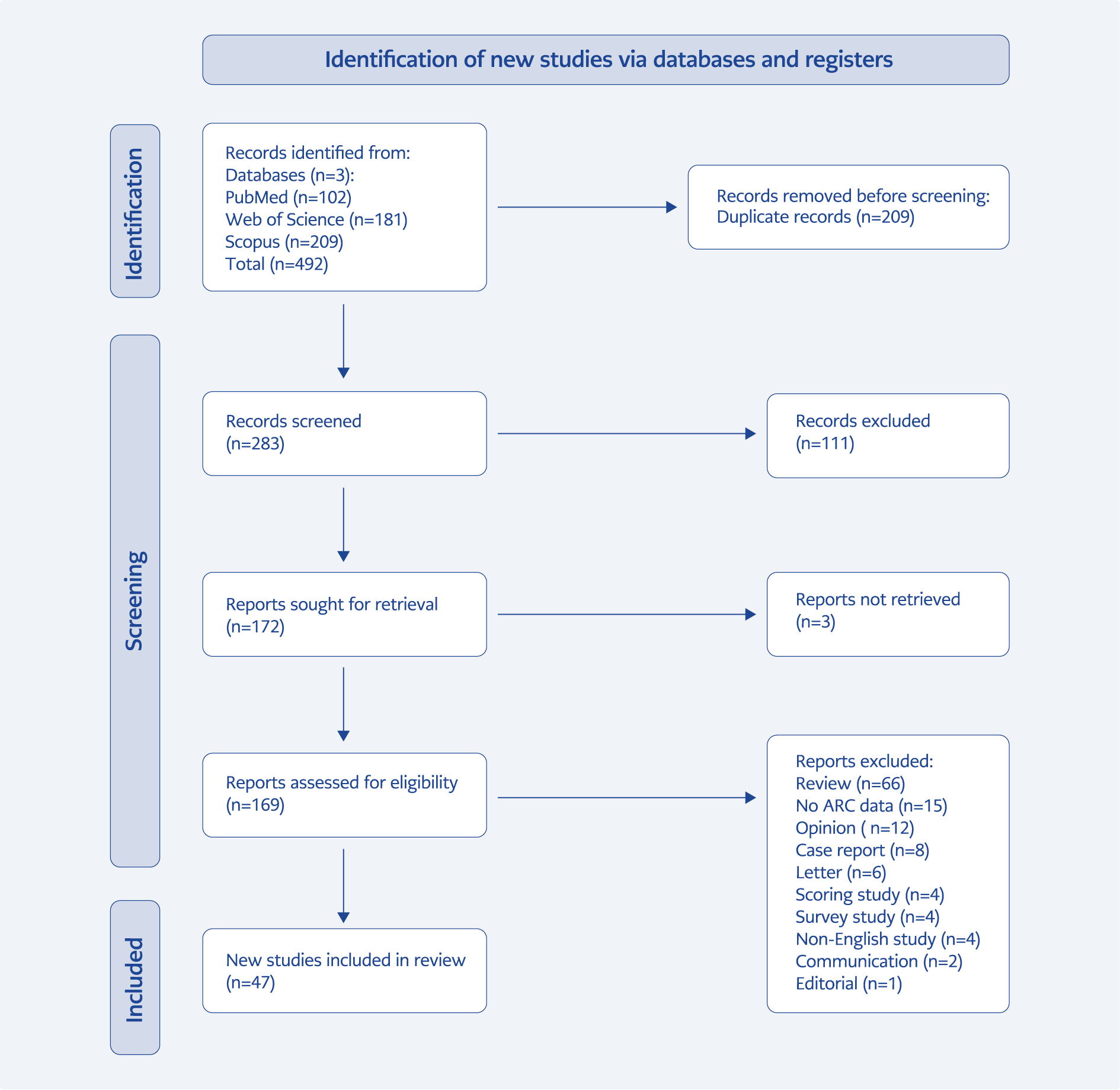
The Rayyan® software (Rayyan Systems Inc., Doha, Qatar) was used to identify duplicates, assess the findings by two independent reviewers (HM and AC), and resolve conflicts between the two reviewers in the presence of a third reviewer. There were two stages to the article selection process. First, duplicates between the three databases were identified and removed. Based on the inclusion and exclusion criteria, the abstracts and titles of the articles were examined. The inclusion criteria were set as follows: the sample age greater than 18 years, the antibacterial drug usage, and the existence of ARC. The exclusion criteria were as follows: non-English language, non-ARC articles, reviews, letters, case reports, opinions, editorials, survey or scoring studies, commentaries, non-human studies, and pediatric population. After the inclusion and exclusion criteria were defined, two reviewers found the full texts of the appropriate articles, and conflicts were resolved. A reviewer was not blinded to the author’s or journal’s names. Figure 1 illustrates the flowchart of the article selection process. The summary of these studies was extracted following the determination of the final full texts.
Data Extraction and Analysis
To analyze the selected articles, the following information was extracted and reviewed by HM, AC, and AP: 1) publication year, 2) the journal name, 3) the aim of the study, 4) study design, 5) sample size and 6) outcomes of the study. Data extraction and tabulation were performed using Microsoft Excel® for Mac, version 16.79.1 (Microsoft Corporation, WA, USA).
Results
A total of 494 articles were identified after the removal of duplicates. Figure 1 shows the PRISMA flowchart. After screening the titles and abstracts, 172 potentially relevant full-text articles were retrieved for further evaluation. After full texts were reviewed, 47 articles met the inclusion criteria and were included in the final analysis (see Supplementary Material). The most common reason for exclusion was that the articles were review studies (n=66), followed by the absence of ARC-related data (n=15). The interrater agreement during full-text selection was substantial, with an agreement rate of 0.87 and a kappa coefficient of 0.751 (95% confidence interval [CI]: 0.614–0.882), according to the classification by Landis et al. (24).
Research Question 1: What are the main characteristics of ARC studies in adult patients receiving antimicrobials?
A total of 47 articles covering 6193 patients were included in this scoping review. The majority of the articles were published in 2022 (29.8%) and had a retrospective observational study design (40.4%). Most of the patients were critically ill, and the mean/median age ranged between 29 and 88 years across studies. Only 21 (44.7%) studies included a critical illness severity score. The top three most reported critical illness severity scores were Acute Physiology and Chronic Health Evaluation II (APACHE II) (n=10, 21.3%), Sequential Organ Failure Assessment (SOFA) (n=12, 25.5%), and Simplified Acute Physiology Score II (SAPS II) (n=5, 10.6%).
Research Question 2: What is the definition, prevalence, and risk factors of ARC in adult patients receiving antimicrobials?
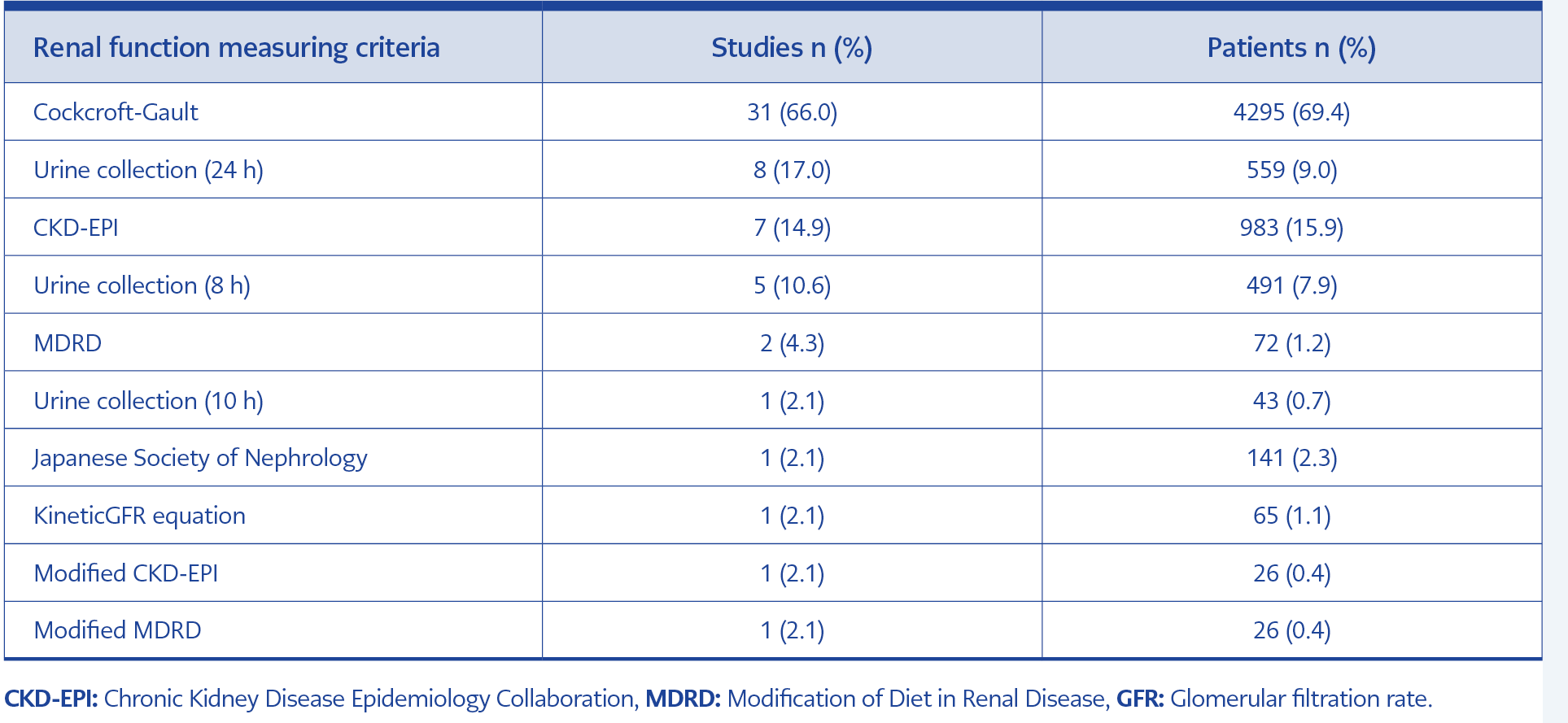
Table 1. The distribution of the studies according to the reported renal function measuring criteria.
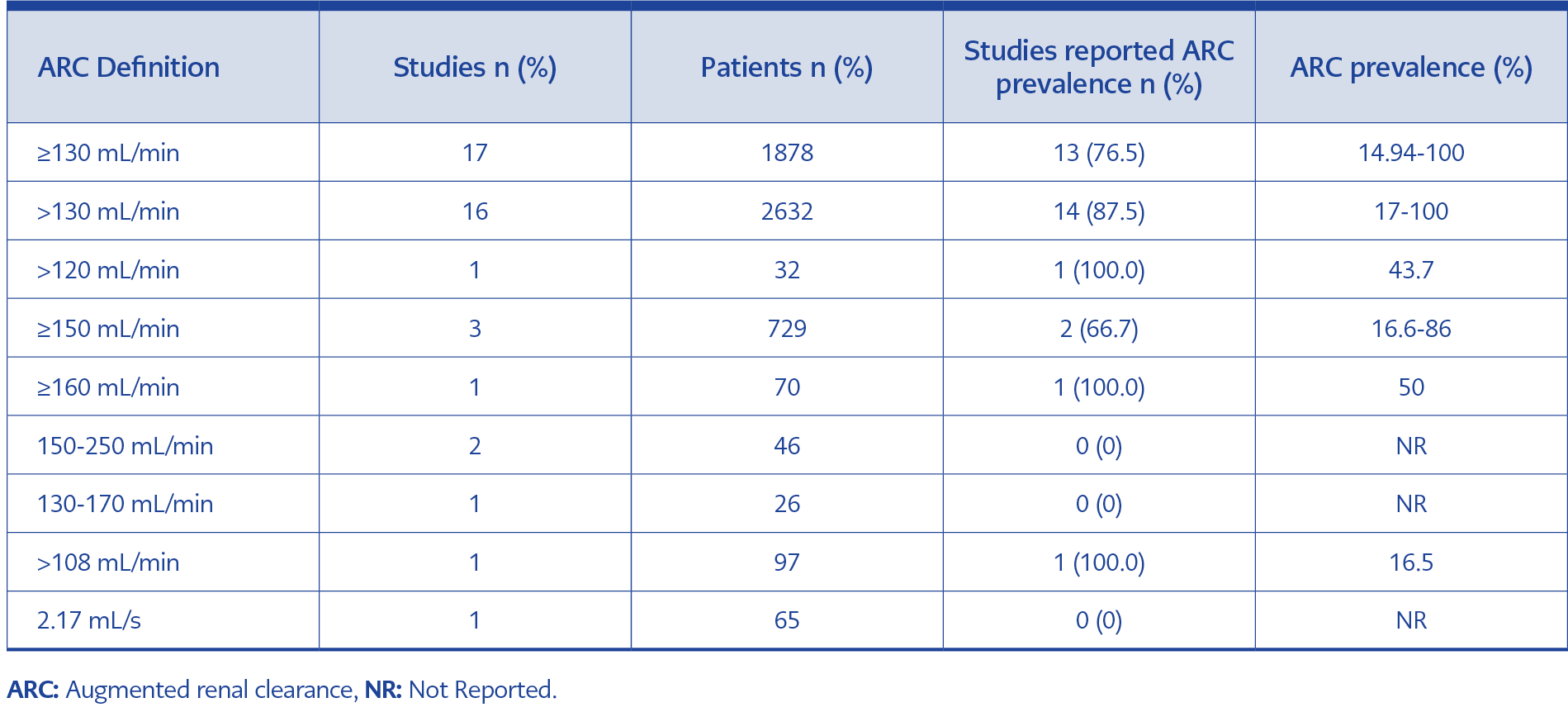
Table 2. The distribution of the studies according to the reported definition and prevalence of ARC.
Across the included studies, CrCl was documented mostly using a modified Cockcroft-Gault equation (52.5%) (Table 1). The ARC prevalence across all studies was between 3.3% and 100%. A summary, including the definition of ARC, the CrCl estimation or determination method, and the prevalence of ARC, is described in Table 2. Of the 47 studies that provided a definition, there were nine distinct definitions of ARC. The most adopted definition of the ARC (in 36.2% of the studies) was CrCl ≥130 mL/min/1.73 m2. Only 8.5% (n=4) of studies evaluated risk factors for ARC, which included age under 50 years (n=2), high body weight (n=2), albumin level (n=1), infection (n=1), gestation age (n=1), enteral nutrition (n=1), male sex (n=1), hypertriglyceridemia (n=1), mechanical ventilation support (n=1), and body mass index (n=1).
Research Question 3: Are there recommended approaches to minimize the effect of ARC on antimicrobial levels in adults?
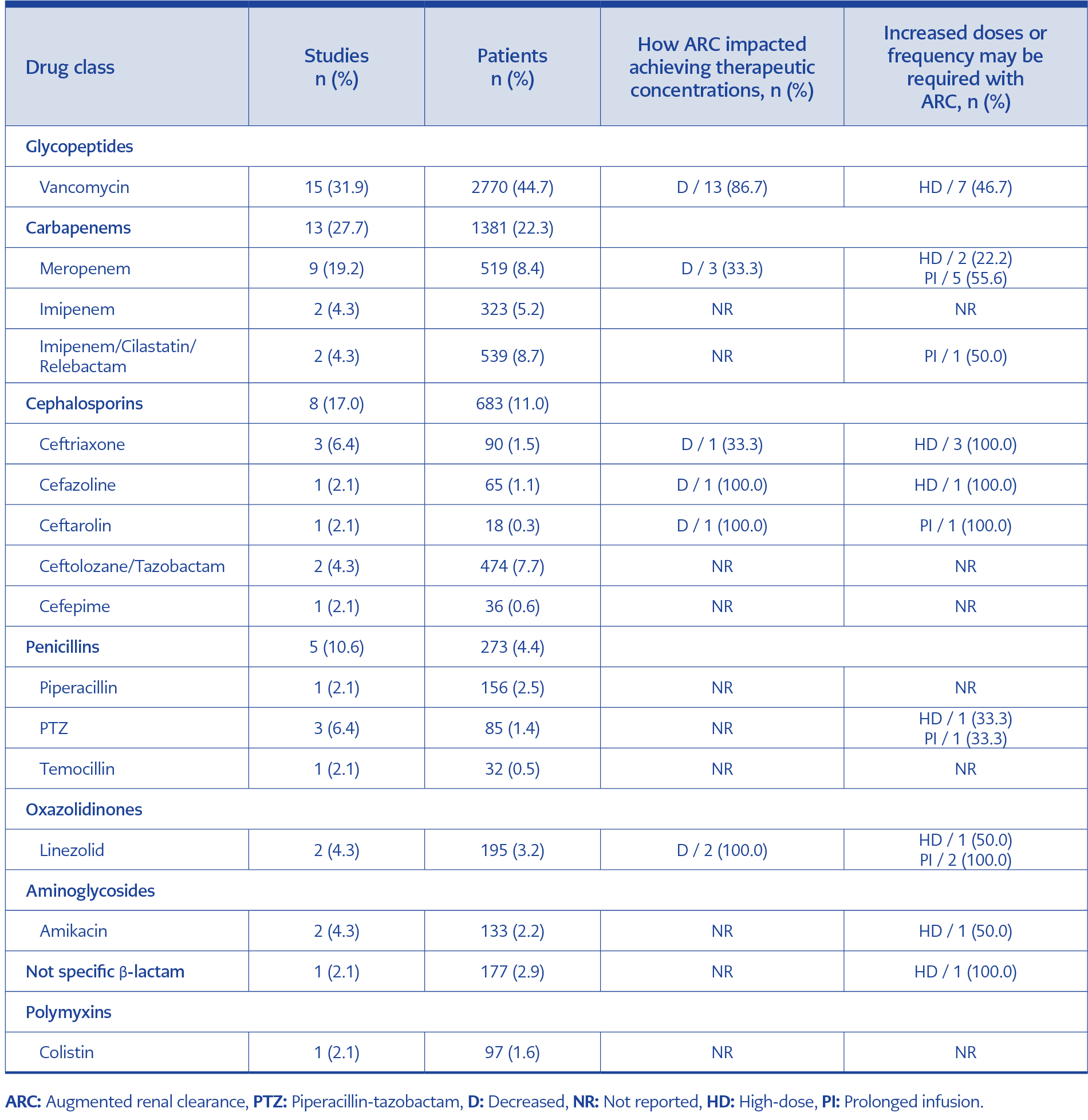
Table 3. The distribution of the studies according to the specific drugs that evaluated the effect of ARC on achieving therapeutic concentrations.
Table 3 summarizes the impact of ARC on achieving therapeutic concentrations of various antibiotic classes and highlights the dosing strategies recommended to address these effects. Glycopeptides, particularly vancomycin, were the most frequently studied group (31.9% of studies), with 86.7% reporting reduced therapeutic concentrations and 46.7% recommending high-dose (HD) administration. Carbapenems (27.7% of studies) showed reduced therapeutic concentrations for meropenem in 33.3% of studies, with 55.6% recommending prolonged infusion (PI). Cephalosporins (17.0%) and penicillins (10.6%) were also commonly evaluated, with some agents requiring HD or PI strategies to counteract ARC-related suboptimal concentrations. Other notable findings included 100% PI recommendations for linezolid and 50% HD recommendations for amikacin. Overall, HD or PI strategies were recommended in 55.3% of studies to mitigate the impact of ARC on therapeutic efficacy.
Research Question 4: What are the gaps for future research?
Most of the included studies are retrospective observational studies, which limit their generalizability. Additionally, in these studies, there needs to be a consensus on the definition of ARC and the criteria for assessing renal function in adult patient populations receiving antimicrobial therapy, making it difficult to compare study results. Only four studies identified risk factors for ARC in adult patients on antimicrobial therapy, highlighting the need for more robustly designed studies to establish these risk factors.
Discussion
A scoping review is a technique employed to identify exhaustive and in-depth literature that has been gathered from various sources using various research methods and is pertinent to the research topic (25). This scoping review analyzed 47 articles related to ARC. Most articles suggest that an increased dosage of antimicrobial agents may be necessary in patients experiencing ARC because of changes in pharmacokinetics and pharmacodynamics.
In the literature, the majority of studies on ARC were conducted on critically ill patients (70.2%). Critically ill patients are at risk for ARC, which is characterized by increased renal function, leading to increased CrCl and drug excretion through the kidneys (6, 26). In a study, approximately half of the intensive care unit (ICU) patients receiving antibiotics exhibited ARC, and the ARC group showed more therapeutic failure (16). Furthermore, antibiotic resistance may be fostered by subtherapeutic dosing (17). In a review examining the effect of ARC on antimicrobial dosing in critically ill pediatric patients, it has been reported that there is an increased drug clearance and, therefore, a lower likelihood of attaining target antibiotic levels (18). This has been associated with reducing drug concentrations below the therapeutic level, potentially leading to therapeutic failure (27). Although a CrCl greater than or equal to 130 mL/min/1.73 m² is the most common definition of ARC, it is also not a standard cut-off for ARC patients (8). In this review, nine different definitions of ARC were obtained. Similarly, a scoping review focusing on ARC in pediatric patients stated that 10 different definitions were given for ARC (18).
According to the findings of this study, the prevalence of ARC varies between 3.3% and 100%. In recent years, there has been a growing recognition of the prevalence of ARC in those who are critically ill. Studies have reported a prevalence of ARC ranging between 28% and 65% in the critical care setting (28). In a scoping review of ARC in critically ill pediatric patients, the prevalence of ARC was between 7.8% and 78% (18). According to the results of another systematic review by Bilbao-Mesequer et al. (8), the prevalence of ARC was stated to be between 20% and 65%.
In critically ill patients, ARC is associated with various risk factors. In this review, ARC risk factors were mentioned in 4 of 47 (8.5%) studies (24, 29-32). According to the results of these studies, age <50 years, albumin level, high body weight, infection, gestational age, enteral nutrition, male sex, hypertriglyceridemia, mechanical ventilation support, and body mass index are among the positive risk factors. Similarly, in the literature, young age, male gender, less severe diseases, trauma, burns, sepsis, and hematological malignancies are found as risk characteristics for ARC (21, 26, 28, 33-37).
Antimicrobial dosing in the context of ARC poses a significant challenge in critically ill patients. ARC can result in suboptimal exposure to antimicrobials, such as β-lactams and vancomycin, thus potentially increasing the risk of unsuccessful treatment (26). Antimicrobial treatment failures have been reported in patients with ARC, highlighting the need to optimize dosing strategies in this population (6). Patients with trauma, sepsis, and neuropathic injury are more likely to develop ARC, making tailored dosing regimens vital for therapeutic success (18). Patients with ARC may face the risk of underdosing with β-lactams, underscoring the need to adjust doses to accommodate enhanced renal clearance (39).
The association between ARC and low plasma levels of administered antimicrobials emphasizes the importance of monitoring drug levels and adjusting dosages accordingly (40). The optimal dosing of antimicrobial agents in critically ill patients with ARC is crucial to achieving effective drug concentrations and improving clinical outcomes (41). The effects of enhanced renal clearance upon treatment failure may require higher total daily doses of antimicrobials in patients with ARC (42). Despite these important findings, this condition is often overlooked in critically ill patients, and treatment outcomes can only be improved by early diagnosis and appropriate management. Individualization of drug doses is necessary when ARC is confirmed, and therapeutic drug monitoring (TDM) is recommended (43).
Of the 47 studies reviewed in this study, 15 were related to vancomycin (31.9%), 13 to carbapenems (27.7%), and eight to cephalosporins (17.0%). ARC patients failed to reach the target therapeutic concentration for vancomycin in 13 of 15 studies, meropenem in three of 13, and cephalosporins in three of 8. Vancomycin studies recommend only increasing the dose, while carbapenem and cephalosporin studies recommend increasing the dose or applying PIs. The study shows that the hydrophilic nature of these three groups of drugs could lead to increased renal elimination in patients with ARC, and thus, increasing their doses and/or prolonging the infusion durations may be a reasonable approach to achieving target levels.
Our findings highlight the importance of individualized dosing strategies in ARC patients, mainly when antibiotics with narrow therapeutic indices or time-dependent pharmacodynamics are used. While dose escalation may be sufficient for vancomycin, prolonging or continuous infusions appear to be a more effective strategy for time-dependent antibiotics like carbapenems and cephalosporins, thus ensuring optimal therapeutic outcomes and minimizing the risk of treatment failure. This was supported by a recent cohort study showing that prolonged β-lactam infusions reduced mortality in patients with bloodstream infections caused by organisms with reduced susceptibility (44). An additional recommended strategy for this patient group is the recommendation of an individual dose through TDM. The administration of high doses of these drugs may result in side effects such as neurotoxicity (β-lactams) and nephrotoxicity (vancomycin). Therefore, plasma drug concentrations must be carefully monitored during treatment (43).
There is a need to explore these strategies further so that standardized protocols can be established for the management of ARC patients in various clinical settings in the future. Research should be conducted in the future to assess the prevalence, identify risk factors, and develop strategies to optimize drug dosing regimens for patients with ARC (45). Healthcare providers can improve clinical outcomes in critically ill patients by addressing the challenges posed by ARC.
This review has some limitations that were reported in other scoping reviews (18, 38). First, some relevant literature may have been missed even though the search was conducted using multiple databases and unrestricted search terms. Secondly, the quality and completeness of the data reported across studies varied, making it challenging to synthesize the findings. For this reason, the scoping review method was selected. Despite these limitations, this review maps the current evidence on antimicrobial dosing in ARC patients and highlights critical research gaps. Notably, this study is the first to provide dosage adjustment recommendations for antimicrobial drug groups by synthesizing the current literature in adult patients with ARC receiving antimicrobial therapy.
In conclusion, our study supports that β-lactams and linezolid may necessitate extended infusion and/or higher dosages to attain therapeutic concentrations in adult ARC patients. Moreover, glycopeptides and aminoglycosides may require higher dosages. Nonetheless, insufficient data exist to recommend a dosage of polymyxins for adult ARC patients.