Introduction
Eosinophilic cellulitis (EC) is a rare inflammatory skin condition with fewer than 200 documented cases in the medical literature (1). There are only a limited number of case reports available from our country. The prevalence and incidence of EC are unknown. The disease is characterized by pruritic, non-purulent, erythematous plaques, with histological findings of edema and eosinophil infiltration in the dermis (2). In some patients, systemic signs such as fever, fatigue, and arthralgia may accompany the condition (3, 4). Some infections, insect bites, medications, and malignancies have been described as possible causative factors of this disease (5-9). It differs from infectious cellulitis by being unresponsive to antibiotics and recurring (1).
This case report presents a late-diagnosed “eosinophilic cellulitis” in a patient with a hematological malignancy who did not respond to long-term, broad-spectrum antibiotics.
Case
A 58-year-old woman with a history of Langerhans cell histiocytosis (LCH) 9 years ago and recurrent LCH 3 years ago presented with redness and fever around the right eye. The patient reported presenting to another hospital with similar complaints 20 days ago, where she was diagnosed with ophthalmic herpes zoster and cellulitis. Subsequently, intravenous treatments with sulbactam-ampicillin (SAM) and acyclovir were initiated. Similar skin lesions developed around the other eye on the sixth day of SAM treatment, and linezolid (LNZ) was added to the treatment. Acyclovir treatment was switched to ganciclovir due to concerns about resistance. The patient, who did not respond to LNZ and SAM, had her treatment revised to include daptomycin (DA) and meropenem (MEM) on the sixth day of LNZ treatment. A skin biopsy on day 20 of her hospitalization was concluded as “diffuse mixed inflammatory cell infiltration rich in perifollicular neutrophils.”
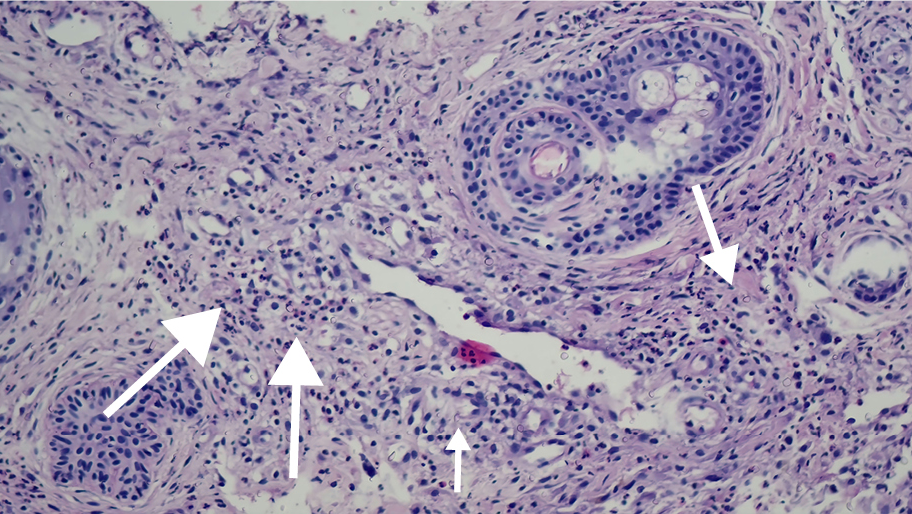
The patient was voluntarily discharged from that hospital and admitted to our center. On physical examination, she exhibited diffuse hyperemia around the right eye and erythematous annular indurated plaques on the right frontal region (Figure 1). Her vital signs were stable. Blood cultures were performed, and initial laboratory studies revealed the following: C-reactive protein (CRP) 107 mg/L, white blood cell (WBC) count 24,500/mm3 [1.8% eosinophil, eosinophil count 400/mm3 (range=0.03-0.27)]. SAM and valacyclovir were initiated. We wondered if the lesions were caused by skin involvement of LCH. A skin biopsy was performed because she did not respond to broad-spectrum antibiotics at the external center. On the fourth day of treatment, preseptal cellulitis was detected in the magnetic resonance imaging of the orbit, leading to a revision of the treatment plan to include DA and piperacillin-tazobactam. Fluconazole was also started for the fungal infection due to the lack of response to broad-spectrum antibiotics. The skin biopsy was performed on day 10 of antibiotic therapy and day 6 of antifungal therapy. The biopsy results included findings of an orthokeratotic stratum corneum, focal hypergranulosis, spongiosis, exocytosis, basal vacuolar degeneration, mononuclear inflammatory cell infiltration, including eosinophils in the dermal layer around the vessels, and on the vessel walls, as well as extravasated erythrocytes. No basal membrane thickening was observed using the histochemical periodic acid-Schiff (PAS) stain method, and there was no evidence of a slight increase in dermal mucin with alcian blue staining. Immunohistochemical assays for CD14, CD68, and S-100 yielded nonspecific results. These findings were interpreted as consistent with EC (Figure 2). Thereupon, the antimicrobial treatment of the patient was discontinued. The patient was given 40 mg/kg/day of systemic prednisolone for three days. Her lesions were significantly regressed on day 3 of the treatment (Figure 3). She was discharged with full recovery and prescribed a maintenance treatment with oral and topical steroids. The CRP level measured 130 mg/L on the initial day of treatment, and it decreased to 8 mg/L by the 12th day of steroid therapy. A high WBC count (27,100/mm3) was considered to be compatible with the use of steroids.
Discussion
Eosinophilic cellulitis, also known as Wells’ syndrome, was first described by Wells in 1971 (2). It is an acute, pruritic, and recurrent dermatitis similar in appearance to infectious cellulitis (1, 2). Antibiotic treatment is frequently administered, often leading to the misdiagnosis of infectious cellulitis (1, 11, 12).
Studies have described various clinical forms characterized by urticarial, vesiculobullous, nodular, papulonodular, annular, and semicircular lesions (7). Lesions can appear as either focal or diffuse, with the most frequent sites being the trunk and extremities, although they may also manifest on the facial area, eyelids, ears, scalp, and other sites (1). Our case was also diagnosed with ophthalmic zona infection, presenting with vesicular-annular erythematous indurated plaques around the right eye.
Eosinophilic cellulitis typically develops within 2-3 days and resolves within 2 to 8 weeks, leaving transient pigmentation without scarring (13).
Common laboratory abnormalities include peripheral eosinophilia, leukocytosis, and elevated erythrocyte sedimentation rate and CRP levels. Cases with normal, moderately high, and elevated CRP and WBC levels have been reported in the literature. Notably, in cases characterized by high CRP and WBC levels that do not respond to antibiotics, significant reductions in CRP levels have been observed following treatment with antihistamines and steroids. (1, 2, 6, 11, 14). In our case, CRP levels, which were high despite broad-spectrum antibiotics, returned to normal after steroid treatment. Eosinophilia has been reported in 50% of cases (12). In this case report, the eosinophil count was 400/mm3 (reference range=30-270/mm3).
The etiopathogenesis of the disease is not fully elucidated. It has been associated with various factors such as excessive eosinophilic activation, hematological malignancies, insect bites, drug use, and infections (viral, bacterial, fungal, parasitic) (7-9). There was a recurrence of LCH in our case.
Eosinophilic cellulitis is distinguished from other eosinophilic dermatoses by the characteristic histopathological findings (eosinophilic infiltration of the dermis, characteristic flame figures, and absence of vasculitis) (14). In our case, the biopsy showed dermal eosinophilic infiltration and flame figures.
Non-steroidal anti-inflammatory drugs (NSAIDs), antihistamines, topical and systemic corticosteroids can be used for the treatment of EC (1). In our case, the response to systemic steroid treatment was dramatic.
In conclusion, this case demonstrates the importance of skin biopsy and histopathological diagnosis. In patients with recurrent, non-purulent, antibiotic-resistant, and infectious cellulitis-like clinical features, “eosinophilic cellulitis” should be kept in mind for the differential diagnosis.